4.1 Layers of the Skin
Learning Objectives
By the end of this section, you will be able to:
- Identify the components of the integumentary system
- Describe the layers of the skin and the functions of each layer
- Identify and describe the hypodermis and deep fascia
- Describe the role of keratinocytes and their life cycle
- Describe the role of melanocytes in skin pigmentation
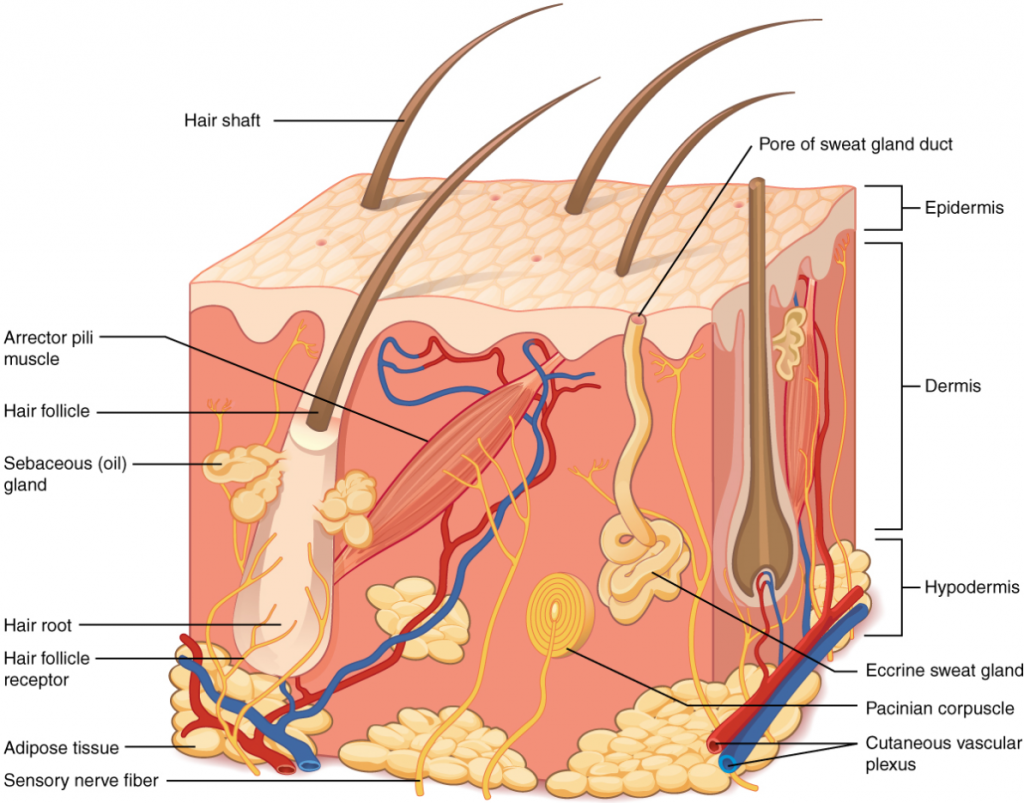
Although you may not typically think of the skin as an organ, it is in fact made of tissues that work together as a single structure to perform unique and critical functions. The skin and its accessory structures make up the integumentary system, which provides the body with overall protection. The skin is made of multiple layers of cells and tissues, which are held to underlying structures by connective tissue (Figure 4.1.1). The deeper layer of skin is well vascularised (has numerous blood vessels). It also has numerous sensory, and autonomic and sympathetic nerve fibres ensuring communication to and from the brain.
The Epidermis
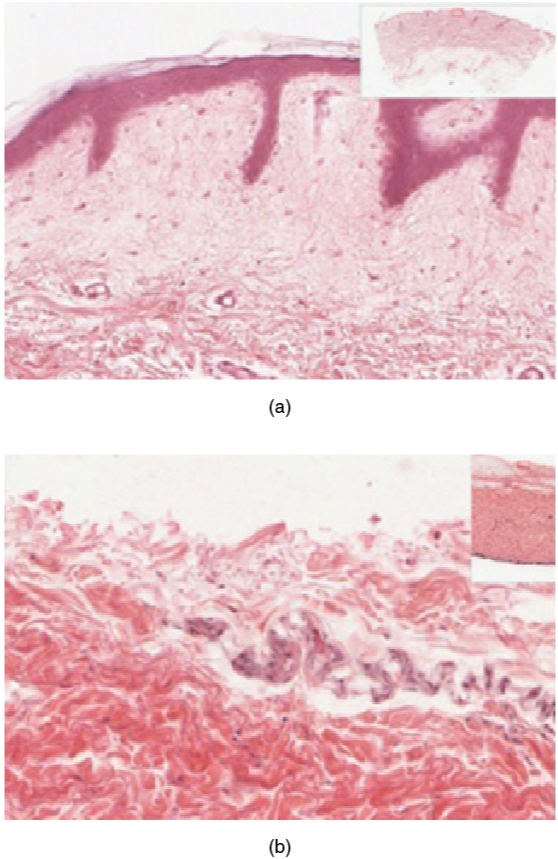
The epidermis is composed of keratinised, stratified squamous epithelium. It is made of four or five layers of epithelial cells, depending on its location in the body. It does not have any blood vessels within it (i.e., it is avascular). Skin that has four layers of cells is referred to as “thin skin.” From deep to superficial, these layers are the stratum basale, stratum spinosum, stratum granulosum, and stratum corneum. Most of the skin can be classified as thin skin. “Thick skin” is found only on the palms of the hands and the soles of the feet. It has a fifth layer, called the stratum lucidum, located between the stratum corneum and the stratum granulosum (Figure 4.1.2).
The cells in all of the layers except the stratum basale are called keratinocytes. A keratinocyte is a cell that manufactures and stores the protein keratin. Keratin is an intracellular fibrous protein that gives hair, nails, and skin their hardness and water-resistant properties. The keratinocytes in the stratum corneum are dead and regularly slough away, being replaced by cells from the deeper layers (Figure 4.1.3).
Stratum Basale
The stratum basale (also called the stratum germinativum) is the deepest epidermal layer and attaches the epidermis to the basal lamina, below which lie the layers of the dermis. The cells in the stratum basale bond to the dermis via intertwining collagen fibres, referred to as the basement membrane. A finger-like projection, or fold, known as the dermal papilla (plural = dermal papillae) is found in the superficial portion of the dermis. Dermal papillae increase the strength of the connection between the epidermis and dermis; the greater the folding, the stronger the connections made (Figure 4.1.4).
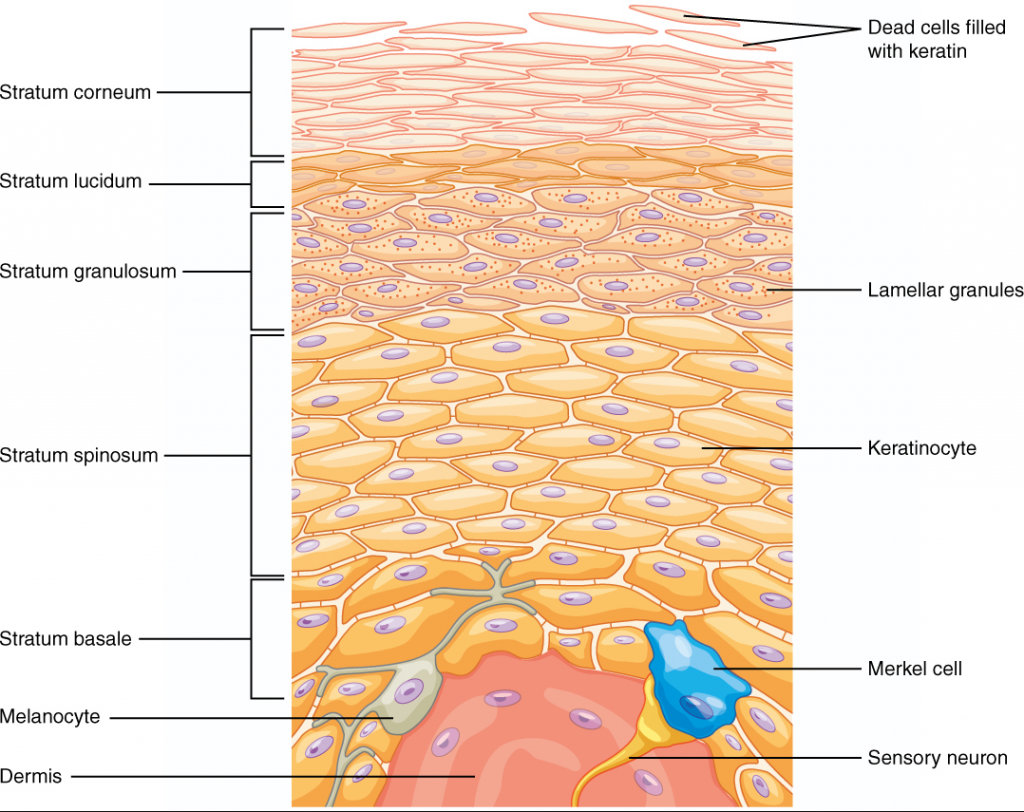
The stratum basale is a single layer of cells primarily made of basal cells. A basal cell is a cuboidal-shaped stem cell that is a precursor of the keratinocytes of the epidermis. All of the keratinocytes are produced from this single layer of cells, which are constantly going through mitosis to produce new cells. As new cells are formed, the existing cells are pushed superficially away from the stratum basale. Two other cell types are found dispersed among the basal cells in the stratum basale. The first is a Merkel cell, which functions as a receptor and is responsible for stimulating sensory nerves that the brain perceives as touch. These cells are especially abundant on the surfaces of the hands and feet. The second is a melanocyte, a cell that produces the pigment melanin. Melanin gives hair and skin its colour, and also helps protect the living cells of the epidermis from ultraviolet (UV) radiation damage.
In a growing foetus, fingerprints form where the cells of the stratum basale meet the papillae of the underlying dermal layer (papillary layer), resulting in the formation of the ridges on your fingers that you recognise as fingerprints. Fingerprints are unique to each individual and are used for forensic analyses because the patterns do not change with the growth and ageing processes.
Stratum Spinosum
As the name suggests, the stratum spinosum is spiny in appearance due to the protruding cell processes that join the cells via a structure called a desmosome. The desmosomes interlock with each other and strengthen the bond between the cells. It is interesting to note that the “spiny” nature of this layer is an artifact of the staining process. Unstained epidermis samples do not exhibit this characteristic appearance. The stratum spinosum is composed of eight to 10 layers of keratinocytes, formed as a result of cell division in the stratum basale (Figure 4.1.5). Interspersed among the keratinocytes of this layer is a type of dendritic cell called the Langerhans cell, which functions as a macrophage by engulfing bacteria, foreign particles, and damaged cells that occur in this layer.
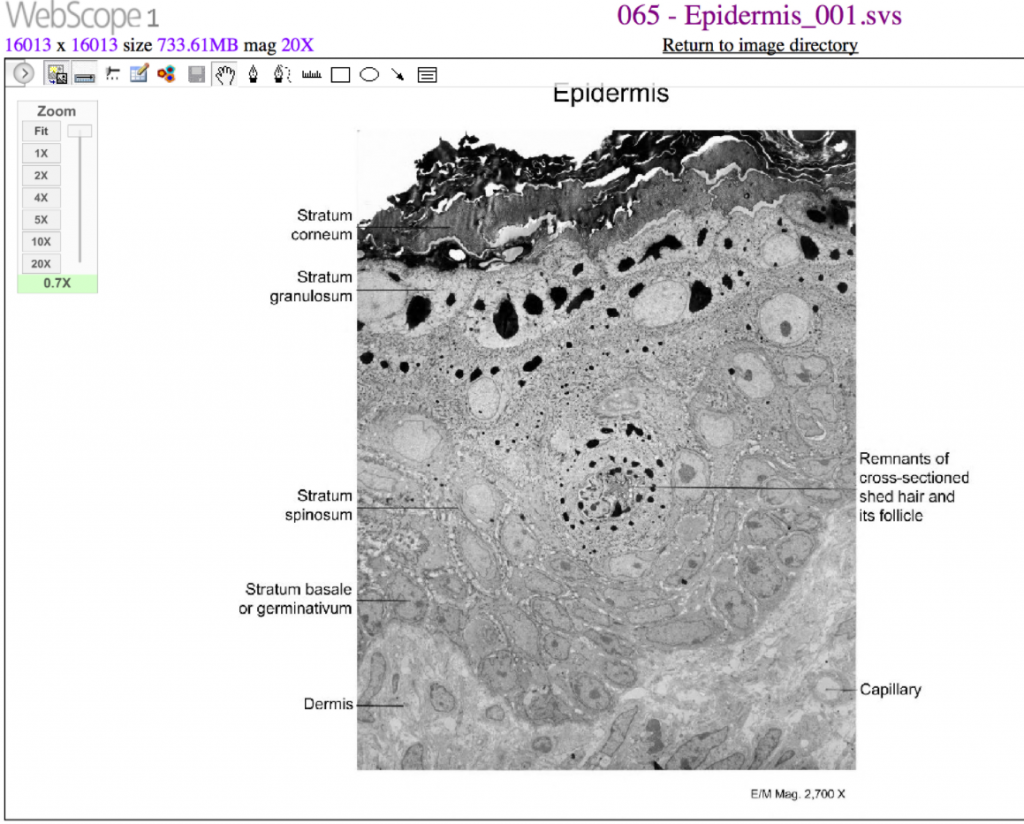
The keratinocytes in the stratum spinosum begin the synthesis of keratin and release a water-repelling glycolipid that helps prevent water loss from the body, making the skin relatively waterproof. As new keratinocytes are produced atop the stratum basale, the keratinocytes of the stratum spinosum are pushed into the stratum granulosum.
Stratum Granulosum
The stratum granulosum has a grainy appearance due to further changes to the keratinocytes as they are pushed from the stratum spinosum. The cells (three to five layers deep) become flatter, their cell membranes thicken, and they generate large amounts of the proteins keratin, which is fibrous, and keratohyalin, which accumulates as lamellar granules within the cells (see Figure 4.1.4 and Figure 4.1.5). These two proteins make up the bulk of the keratinocyte mass in the stratum granulosum and give the layer its grainy appearance. The nuclei and other cell organelles disintegrate as the cells die, leaving behind the keratin, keratohyalin, and cell membranes that will form the stratum lucidum, the stratum corneum, and the accessory structures of hair and nails.
Stratum Lucidum
The stratum lucidum is a smooth, seemingly translucent layer of the epidermis located just above the stratum granulosum and below the stratum corneum. This thin layer of cells is found only in the thick skin of the palms, soles, and digits. The keratinocytes that compose the stratum lucidum are dead and flattened (see Figure 4.1.4 and Figure 4.1.5). These cells are densely packed with eleidin, a clear protein rich in lipids, derived from keratohyalin, which gives these cells their transparent (i.e., lucid) appearance and provides a barrier to water.
Stratum Corneum
The stratum corneum is the most superficial layer of the epidermis and is the layer exposed to the outside environment (see Figure 4.1.4 and Figure 4.1.5). The increased keratinisation (also called cornification) of the cells in this layer gives it its name. There are usually 15 to 30 layers of cells in the stratum corneum. This dry, dead layer helps prevent the penetration of microbes and the dehydration of underlying tissues and provides a mechanical protection against abrasion for the more delicate, underlying layers. Cells in this layer are shed periodically and are replaced by cells pushed up from the stratum granulosum (or stratum lucidum in the case of the palms and soles of feet). The entire layer is replaced during a period of about 4 weeks. Cosmetic procedures, such as microdermabrasion, help remove some of the dry, upper layer and aim to keep the skin looking “fresh” and healthy.
Dermis
The dermis might be considered the “core” of the integumentary system (derma- = “skin”), as distinct from the epidermis (epi- = “upon” or “over”) and hypodermis (hypo- = “below”). It contains blood and lymph vessels, nerves, and other structures, such as hair follicles and sweat glands. The dermis is made of two layers of connective tissue that compose an interconnected mesh of elastin and collagenous fibres, produced by fibroblasts (Figure 4.1.6).

Papillary Layer
The papillary layer is made of loose, areolar connective tissue, which means the collagen and elastin fibres of this layer form a loose mesh. This superficial layer of the dermis projects into the stratum basale of the epidermis to form finger-like dermal papillae (see Figure 4.1.6). Within the papillary layer are fibroblasts, a small number of fat cells (adipocytes), and an abundance of small blood vessels. In addition, the papillary layer contains phagocytes, defensive cells that help fight bacteria or other infections that have breached the skin. This layer also contains lymphatic capillaries, nerve fibres, and touch receptors called the Meissner corpuscles.
Reticular Layer
Underlying the papillary layer is the much thicker reticular layer, composed of dense, irregular connective tissue. This layer is well vascularised and has a rich sensory and sympathetic nerve supply. The reticular layer appears reticulated (net-like) due to a tight meshwork of fibres. Elastin fibres provide some elasticity to the skin, enabling movement. Collagen fibres provide structure and tensile strength, with strands of collagen extending into both the papillary layer and the hypodermis. In addition, collagen binds water to keep the skin hydrated. Collagen injections and Retin-A creams help restore skin turgor by either introducing collagen externally or stimulating blood flow and repair of the dermis, respectively.
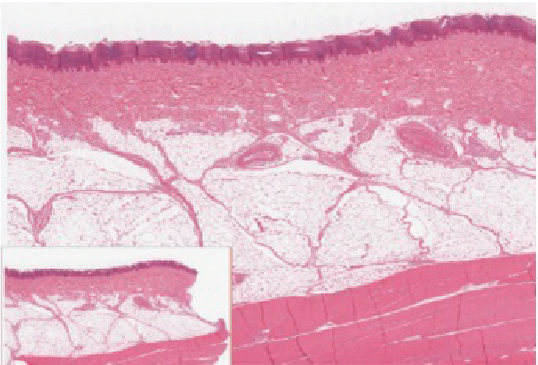
Hypodermis
The hypodermis (also called the subcutaneous layer or superficial fascia) is a layer directly below the dermis and serves to connect the skin to the underlying fascia (fibrous tissue) of the bones and muscles. It is not strictly a part of the skin, although the border between the hypodermis and dermis can be difficult to distinguish. The hypodermis consists of well-vascularised, loose, areolar connective tissue and adipose tissue, which functions as a mode of fat storage and provides insulation and cushioning for the integument.
Everyday Connection
Lipid Storage
The hypodermis is home to most of the fat that concerns people when they are trying to keep their weight under control. Adipose tissue present in the hypodermis consists of fat-storing cells called adipocytes. This stored fat can serve as an energy reserve, insulate the body to prevent heat loss, and act as a cushion to protect underlying structures from trauma.
Where the fat is deposited and accumulates within the hypodermis depends on hormones (testosterone, oestrogen, insulin, glucagon, leptin and others), as well as genetic factors. Fat distribution changes as our bodies mature and age. Men tend to accumulate fat in different areas (neck, arms, lower back, and abdomen) than do women (breasts, hips, thighs, and buttocks). The body mass index (BMI) is often used as a measure of fat, although this measure is, in fact, derived from a mathematical formula that compares body weight (mass) to height. Therefore, its accuracy as a health indicator can be called into question in individuals who are extremely physically fit.
In many animals, there is a pattern of storing excess calories as fat to be used in times when food is not readily available. In much of the developed world, insufficient exercise coupled with the ready availability and consumption of high-calorie foods have resulted in unwanted accumulations of adipose tissue in many people. Although periodic accumulation of excess fat may have provided an evolutionary advantage to our ancestors, who experienced unpredictable bouts of famine, it is now becoming chronic and considered a major health threat. Recent studies indicate that a distressing percentage of our population is overweight and/or clinically obese. Not only is this a problem for the individuals affected, but it also has a severe impact on our healthcare system. Changes in lifestyle, specifically in diet and exercise, are the best ways to control body fat accumulation, especially when it reaches levels that increase the risk of heart disease and diabetes.
Pigmentation
The colour of skin is influenced by a number of pigments, including melanin, carotene and haemoglobin. Recall that melanin is produced by cells called melanocytes, which are found scattered throughout the stratum basale of the epidermis. The melanin is transferred into the keratinocytes via a cellular vesicle called a melanosome (Figure 4.1.7).
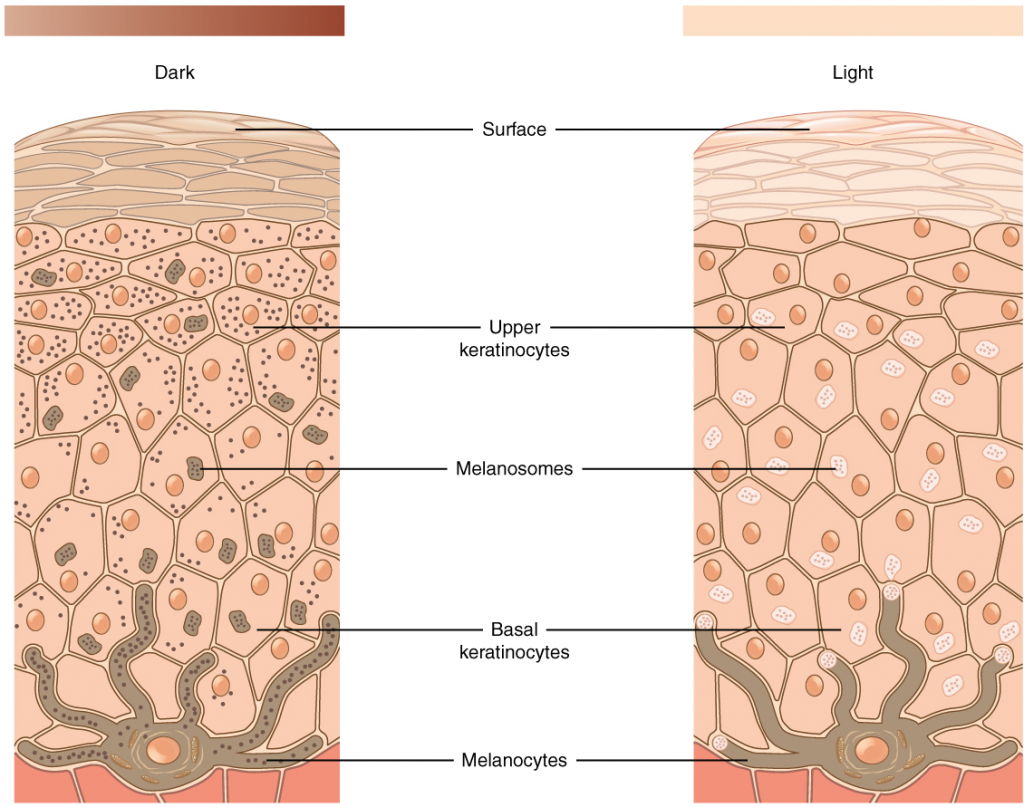
Melanin occurs in two primary forms. Eumelanin exists as black and brown, whereas pheomelanin provides a red colour. Dark-skinned individuals produce more melanin than those with pale skin. Exposure to the UV rays of the sun or a tanning salon causes melanin to be manufactured and built up in keratinocytes, as sun exposure stimulates keratinocytes to secrete chemicals that stimulate melanocytes. The accumulation of melanin in keratinocytes results in the darkening of the skin, or a tan. This increased melanin accumulation protects the DNA of epidermal cells from UV ray damage and the breakdown of folic acid, a nutrient necessary for our health and well-being. In contrast, too much melanin can interfere with the production of vitamin D, an important nutrient involved in calcium absorption. Thus, the amount of melanin present in our skin is dependent on a balance between available sunlight and folic acid destruction, and protection from UV radiation and vitamin D production.
It requires about 10 days after initial sun exposure for melanin synthesis to peak, which is why pale-skinned individuals tend to suffer sunburns of the epidermis initially. Dark-skinned individuals can also get sunburned but are more protected than are pale-skinned individuals. Melanosomes are temporary structures that are eventually destroyed by fusion with lysosomes; this fact, along with melanin-filled keratinocytes in the stratum corneum sloughing off, makes tanning impermanent.
Too much sun exposure can eventually lead to wrinkling due to the destruction of the cellular structure of the skin, and in severe cases, can cause sufficient DNA damage to result in skin cancer. When there is an irregular accumulation of melanocytes in the skin, freckles appear. Moles are larger masses of melanocytes, and although most are benign, they should be monitored for changes that might indicate the presence of cancer (Figure 4.1.8).
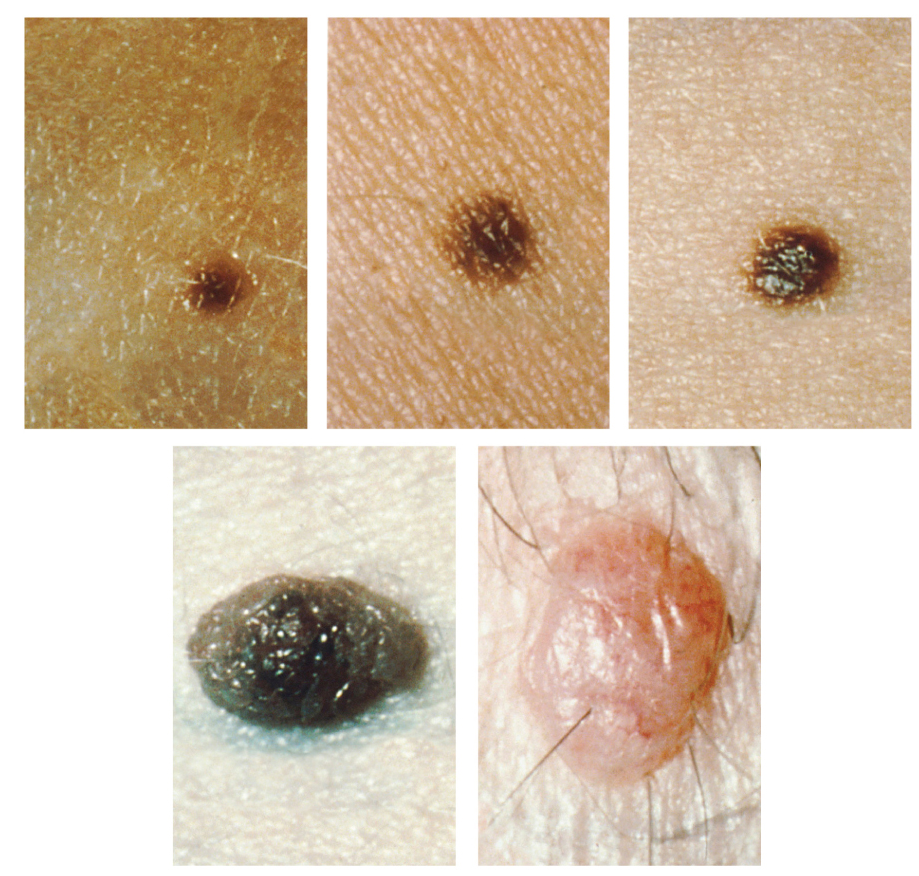
Disorders of the Integumentary System

The first thing a clinician sees is the skin, and so the examination of the skin should be part of any thorough physical examination. Most skin disorders are relatively benign, but a few, including melanomas, can be fatal if untreated. A couple of the more noticeable disorders, albinism and vitiligo, affect the appearance of the skin and its accessory organs. Although neither is fatal, it would be hard to claim that they are benign, at least to the individuals so afflicted.
Albinism is a genetic disorder that affects (completely or partially) the colouring of skin, hair, and eyes. The defect is primarily due to the inability of melanocytes to produce melanin. Individuals with albinism tend to appear white or very pale due to the lack of melanin in their skin and hair. Recall that melanin helps protect the skin from the harmful effects of UV radiation. Individuals with albinism tend to need more protection from UV radiation, as they are more prone to sunburns and skin cancer. They also tend to be more sensitive to light and have vision problems due to the lack of pigmentation on the retinal wall. Treatment of this disorder usually involves addressing the symptoms, such as limiting UV light exposure to the skin and eyes. In vitiligo, the melanocytes in certain areas lose their ability to produce melanin, possibly due to an autoimmune reaction. This leads to a loss of colour in patches (Figure 4.1.9). Neither albinism nor vitiligo directly affects the lifespan of an individual.
Section Review
The skin is composed of two major layers: a superficial epidermis and a deeper dermis. The epidermis consists of several layers beginning with the innermost (deepest) stratum basale (germinatum), followed by the stratum spinosum, stratum granulosum, stratum lucidum (when present), and ending with the outermost layer, the stratum corneum. The topmost layer, the stratum corneum, consists of dead cells that shed periodically and is progressively replaced by cells formed from the basal layer. The stratum basale also contains melanocytes, cells that produce melanin, the pigment primarily responsible for giving skin its colour. Melanin is transferred to keratinocytes in the stratum spinosum to protect cells from UV rays.
The dermis connects the epidermis to the hypodermis and provides strength and elasticity due to the presence of collagen and elastin fibres. It has only two layers: the papillary layer with papillae that extend into the epidermis and the lower, reticular layer composed of loose connective tissue. The hypodermis, deep to the dermis of skin, is the connective tissue that connects the dermis to underlying structures; it also harbors adipose tissue for fat storage and protection.
Review Questions
Critical Thinking Questions
Click the drop down below to review the terms learned from this chapter.

