10.3 Bone Structure
Learning Objectives
By the end of this section, you will be able to:
- Identify the anatomical features of a bone
- Define and list examples of bone markings
- Describe the histology of bone tissue
- Compare and contrast compact and spongy bone
- Identify the structures that compose compact and spongy bone
- Describe how bones are nourished and innervated
Bone tissue (osseous tissue) differs from other tissues in the body. Bone is hard and many of its functions depend on that characteristic hardness. Later discussions in this chapter will show that bone is also dynamic in that its shape adjusts to accommodate stresses. This section will examine the gross anatomy of bone first and then move on to its histology.
Gross Anatomy of Bone
The structure of a long bone allows for the best visualisation of all the parts of a bone (Figure 10.3.1). A long bone has two parts: the diaphysis and the epiphysis. The diaphysis is the tubular shaft that runs between the proximal and distal ends of the bone. The hollow region in the diaphysis is called the medullary cavity, which is filled with yellow marrow. The walls of the diaphysis are composed of dense and hard compact bone.
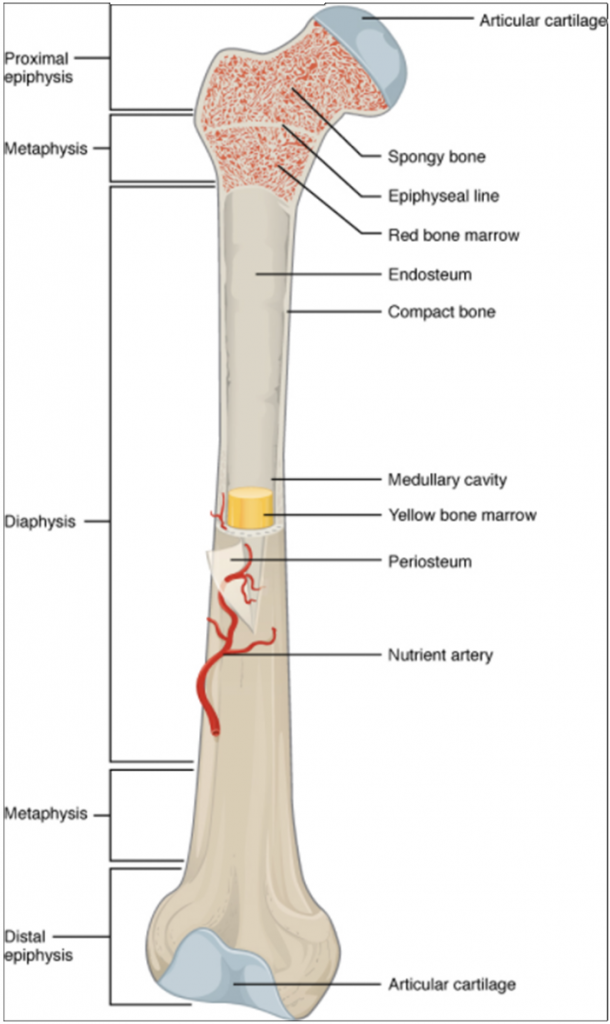
The wider section at each end of the bone is called the epiphysis (plural = epiphyses), which is filled with spongy bone. Red marrow fills the spaces in the spongy bone. Each epiphysis meets the diaphysis at the metaphysis, the narrow area that contains the epiphyseal plate (growth plate), a layer of hyaline (transparent) cartilage in a growing bone. When the bone stops growing in early adulthood (approximately 18–21 years), the cartilage is replaced by osseous tissue and the epiphyseal plate becomes an epiphyseal line.
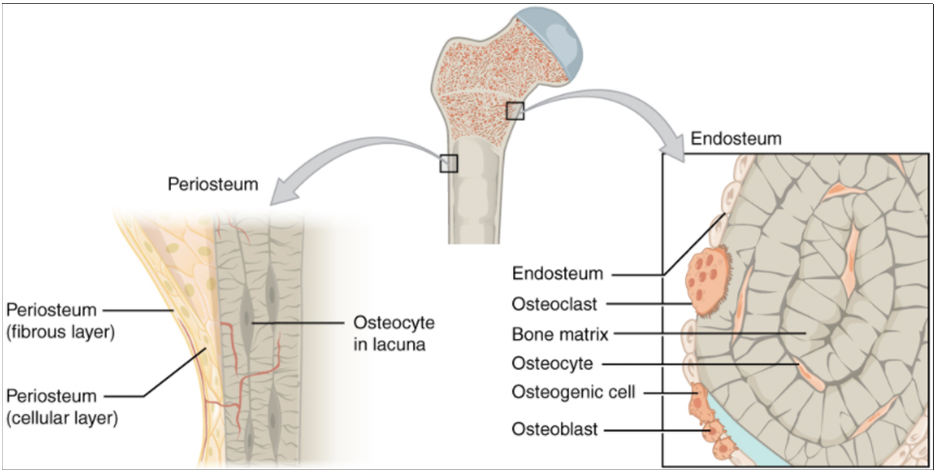
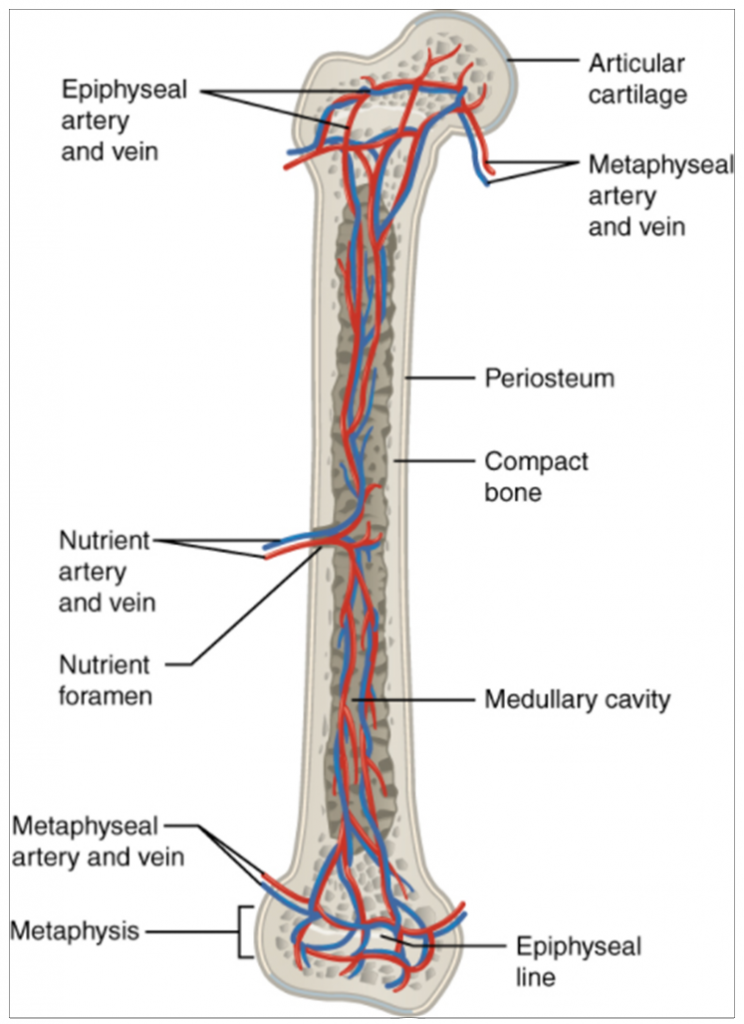
The medullary cavity has a delicate membranous lining called the endosteum (end- = “inside”; oste- = “bone”), where bone growth, repair, and remodelling occur. The outer surface of the bone is covered with a fibrous membrane called the periosteum (peri– = “around” or “surrounding”). The periosteum contains blood vessels, nerves, and lymphatic vessels that nourish compact bone. Tendons and ligaments also attach to bones at the periosteum. The periosteum covers the entire outer surface except where the epiphyses meet other bones to form joints (Figure 10.3.2). In this region, the epiphyses are covered with articular cartilage, a thin layer of cartilage that reduces friction and acts as a shock absorber.
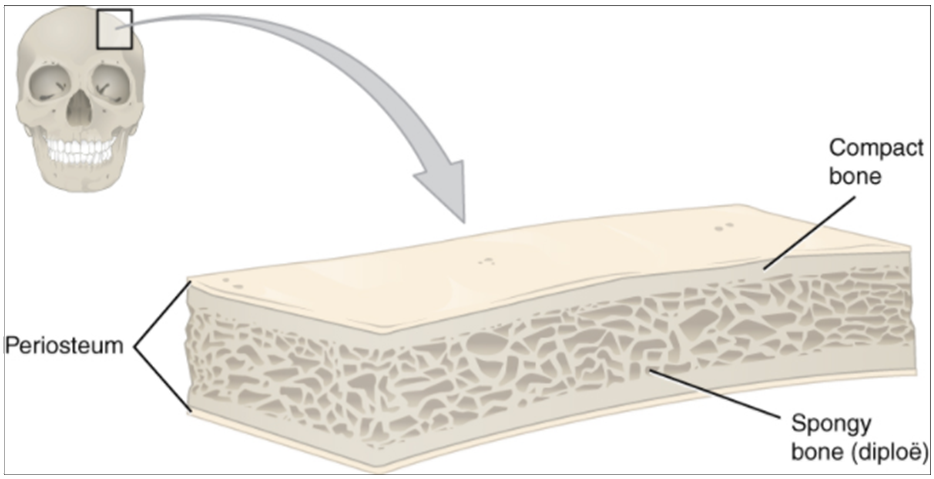
Flat bones, like those of the cranium, consist of a layer of diploë (spongy bone), lined on either side by a layer of compact bone (Figure 10.3.3). The two layers of compact bone and the interior spongy bone work together to protect the internal organs. If the outer layer of a cranial bone fractures, the brain is still protected by the intact inner layer.
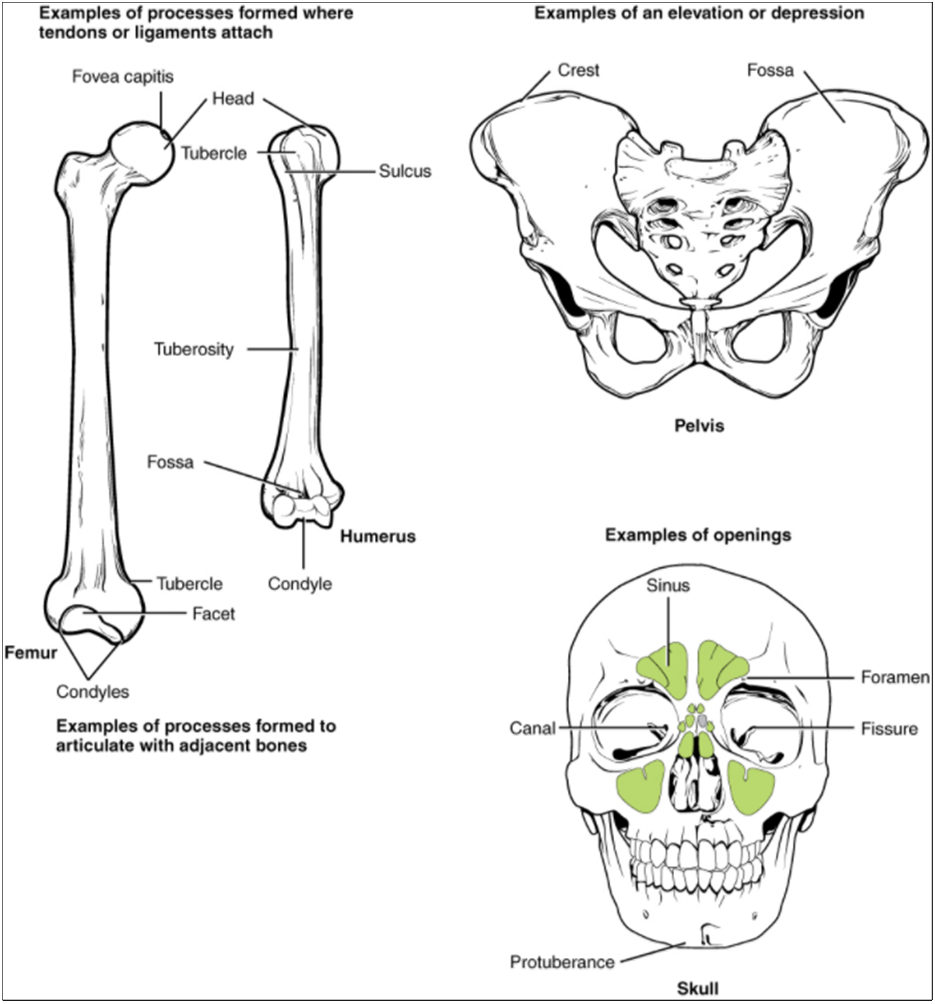
Bone Markings
The surface features of bones vary depending on the function and location in the body. Table 10.3.1 describes the bone markings, which are illustrated in (Figure 10.3.4). There are three general classes of bone markings: (1) articulations, (2) projections and (3) holes. As the name implies, an articulation is where two bone surfaces come together (articulus = “joint”). These surfaces tend to conform to one another, such as one being rounded and the other cupped, to facilitate the function of the articulation. A projection is an area of a bone that projects above the surface of the bone. These are the attachment points for tendons and ligaments. In general, their size and shape are an indication of the forces exerted through the attachment to the bone. A hole is an opening or groove in the bone that allows blood vessels and nerves to enter the bone. As with the other markings, their size and shape reflect the size of the vessels and nerves that penetrate the bone at these points.
Table 10.3.1 Bone Markings
| Marking | Description | Example |
| Articulations | Where two bones meet | Knee joint |
| Canal | Passage in bone | Auditory canal |
| Condyle | Rounded surface | Occipital condyles |
| Crest | Ridge | Iliac crest |
| Facet | Flat surface | Vertebrae |
| Fissure | Slit through bone | Auricular fissure |
| Foramen | Hole through bone | Foramen magnum in the occipital bone |
| Fossa | Elongated basin | Mandibular fossa |
| Fovea | Small pit | Fovea capitis on the head of the femur |
| Head | Prominent rounded surface | Head of femur |
| Holes | Holes and depressions | Foramen (holes through which blood vessels can pass through) |
| Line | Slight, elongated ridge | Temporal lines of the parietal bones |
| Meatus | Opening into canal | External auditory meatus |
| Process | Prominence feature | Transverse process of vertebra |
| Projections | Raised Markings | Spinous process of the vertebrae |
| Protuberance | Protruding | Chin |
| Sinus | Air-filled space in bone | Nasal sinus |
| Spine | Sharp process | Ischial spine |
| Sulcus | Groove | Sigmoid sulcus of the temporal bones |
| Tubercle | Small, rounded process | Deltoid tuberosity |
Bone Cells and Tissue
Bone contains a relatively small number of cells entrenched in a matrix of collagen fibres that provide a surface for inorganic salt crystals to adhere. These salt crystals form when calcium phosphate and calcium carbonate combine to create hydroxyapatite, which incorporates other inorganic salts like magnesium hydroxide, fluoride and sulphate as it crystallises, or calcifies, on the collagen fibres. The hydroxyapatite crystals give bones their hardness and strength, while the collagen fibres give them flexibility so that they are not brittle.
Although bone cells compose a small amount of the bone volume, they are crucial to the function of bones. Four types of cells are found within bone tissue: osteoblasts, osteocytes, osteogenic cells and osteoclasts (Figure 10.3.5).
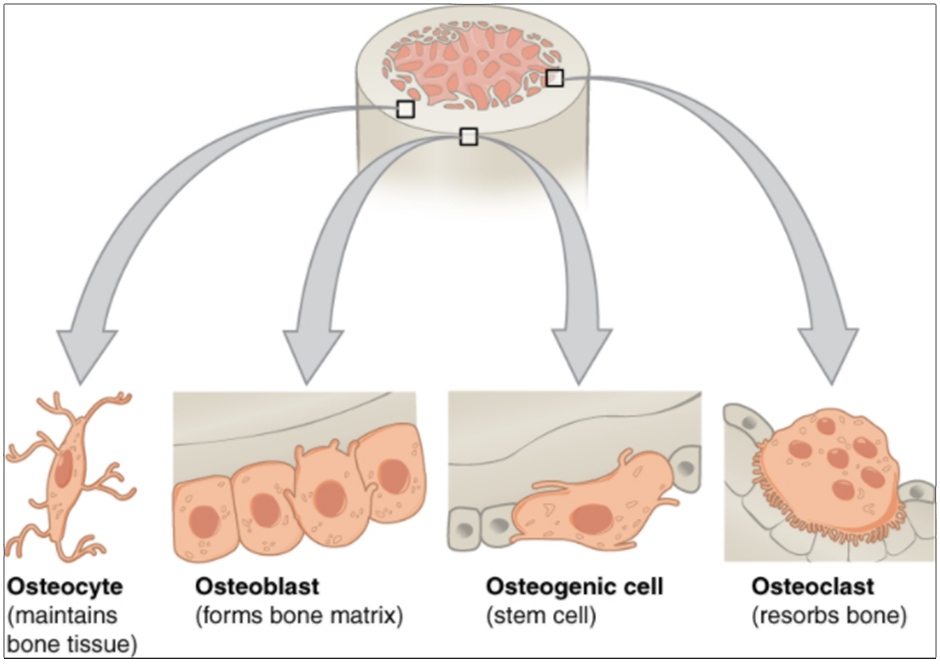
The osteoblast is the bone cell responsible for forming new bone and is found in the growing portions of bone, including the periosteum and endosteum. Osteoblasts, which do not divide, synthesise and secrete the collagen matrix and calcium salts. As the secreted matrix surrounding the osteoblast calcifies, the osteoblast become trapped within it; as a result, it changes in structure and becomes an osteocyte, the primary cell of mature bone and the most common type of bone cell. Each osteocyte is located in a space called a lacuna and is surrounded by bone tissue. Osteocytes maintain the mineral concentration of the matrix via the secretion of enzymes. Like osteoblasts, osteocytes lack mitotic activity. They can communicate with each other and receive nutrients via long cytoplasmic processes that extend through canaliculi (singular = canaliculus), channels within the bone matrix.
If osteoblasts and osteocytes are incapable of mitosis, then how are they replenished when old ones die? The answer lies in the properties of a third category of bone cells—the osteogenic cell. These osteogenic cells are undifferentiated with high mitotic activity and they are the only bone cells that divide. Immature osteogenic cells are found in the deep layers of the periosteum and the marrow. They differentiate and develop into osteoblasts.
The dynamic nature of bone means that new tissue is constantly formed, and old, injured, or unnecessary bone is dissolved for repair or for calcium release. The cell responsible for bone resorption, or breakdown, is the osteoclast. They are found on bone surfaces, are multinucleated, and originate from monocytes and macrophages, two types of white blood cells, not from osteogenic cells. Osteoclasts are continually breaking down old bone while osteoblasts are continually forming new bone. The ongoing balance between osteoblasts and osteoclasts is responsible for the constant but subtle reshaping of bone. Table 10.3.2 reviews the bone cells, their functions and locations.
Table 10.3.2. Bone Cells
| Cell type | Function | Location |
| Osteogenic cells | Develop into osteoblasts | Deep layers of the periosteum and the marrow |
| Osteoblasts | Bone formation | Growing portions of bone, including periosteum and endosteum |
| Osteocytes | Maintain mineral concentration of matrix | Entrapped in matrix |
| Osteoclasts | Bone resorption | Bone surfaces and at sites of old, injured or unneeded bone |
Compact and Spongy Bone
The differences between compact and spongy bone are best explored via their histology. Most bones contain compact and spongy osseous tissue, but their distribution and concentration vary based on the bone’s overall function. Compact bone is dense so that it can withstand compressive forces, while spongy (cancellous) bone has open spaces and supports shifts in weight distribution.
Compact Bone
Compact bone is the denser, stronger of the two types of bone tissue (Figure 10.3.6). It can be found under the periosteum and in the diaphyses of long bones, where it provides support and protection.
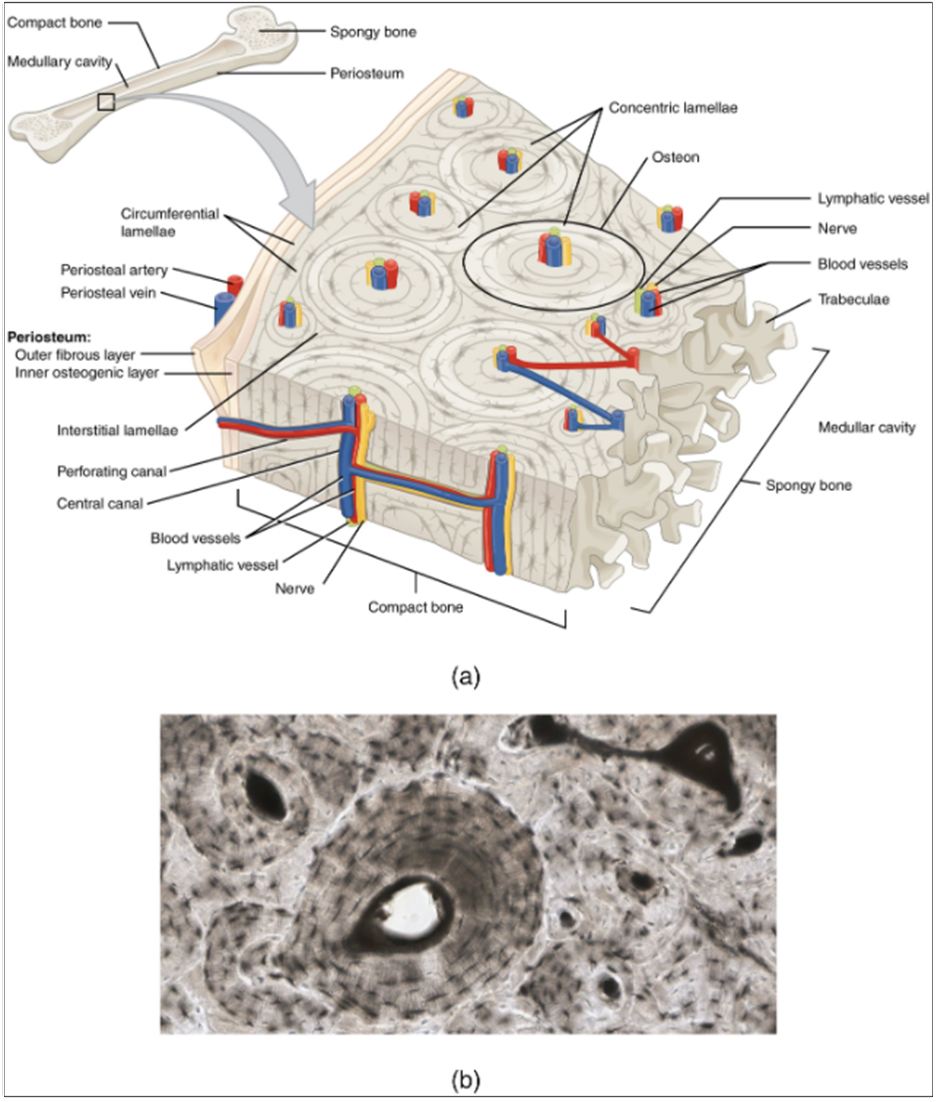
The microscopic structural unit of compact bone is called an osteon, or Haversian system. Each osteon is composed of concentric rings of calcified matrix called lamellae (singular = lamella). Running down the centre of each osteon is the central canal, or Haversian canal, which contains blood vessels, nerves, and lymphatic vessels. These vessels and nerves branch off at right angles through a perforating canal, also known as Volkmann’s canals, to extend to the periosteum and endosteum.
The osteocytes are located inside spaces called lacunae (singular = lacuna), found at the borders of adjacent lamellae. As described earlier, canaliculi connect with the canaliculi of other lacunae and eventually with the central canal. This system allows nutrients to be transported to the osteocytes and wastes to be removed from them.
Spongy (Cancellous) Bone
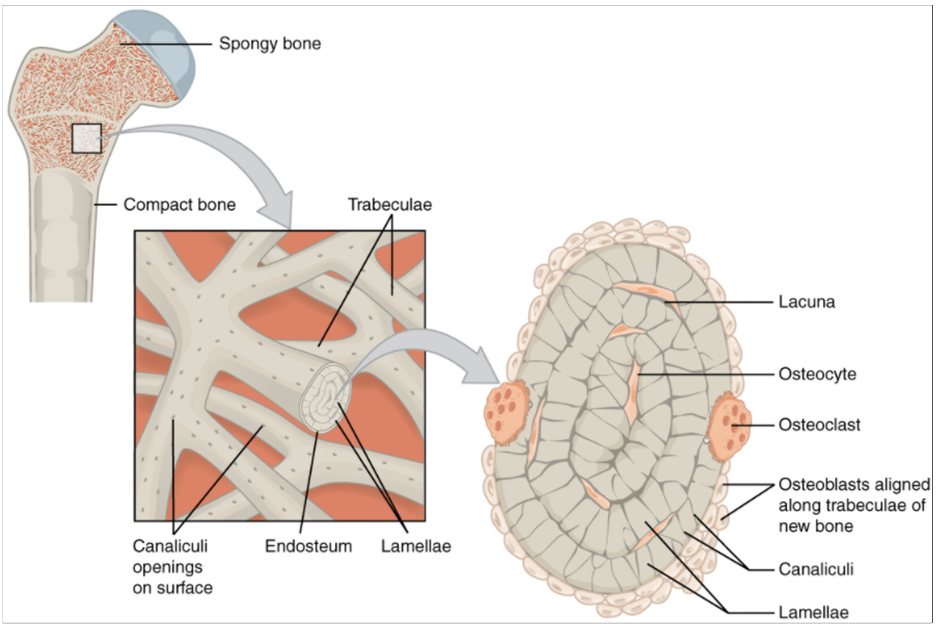
Like compact bone, spongy bone, also known as cancellous bone, contains osteocytes housed in lacunae, but they are not arranged in concentric circles. Instead, the lacunae and osteocytes are found in a lattice-like network of matrix spikes called trabeculae (singular = trabecula) (Figure 10.3.7). The trabeculae may appear to be a random network, but each trabecula forms along lines of stress to provide strength to the bone. The spaces of the trabeculated network provide balance to the dense and heavy compact bone by making bones lighter so that muscles can move them more easily. In addition, the spaces in some spongy bones contain red marrow, protected by the trabeculae, where haematopoiesis occurs.
Ageing and the Skeletal System: Paget’s Disease
Paget’s disease usually occurs in adults over age 40. It is a disorder of the bone remodelling process that begins with overactive osteoclasts. This means more bone is resorbed than is laid down. The osteoblasts try to compensate but the new bone they lay down is weak and brittle and therefore prone to fracture.
While some people with Paget’s disease have no symptoms, others experience pain, bone fractures, and bone deformities (Figure 10.3.8). Bones of the pelvis, skull, spine, and legs are the most affected. When occurring in the skull, Paget’s disease can cause headaches and hearing loss.
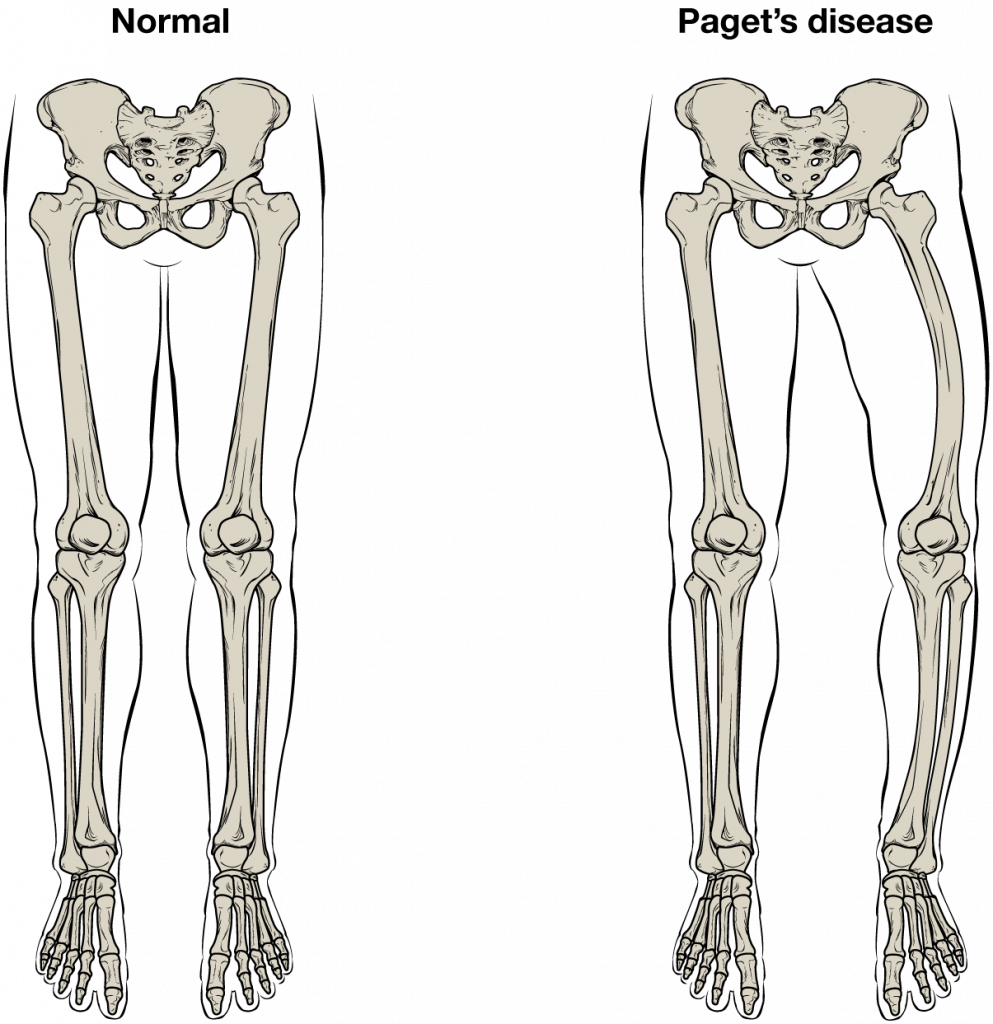
What causes the osteoclasts to become overactive? The answer is still unknown, but hereditary factors play a role. Some scientists believe Paget’s disease is due to an as-yet-unidentified virus.
Paget’s disease is diagnosed via imaging studies and lab tests. X-rays may show bone deformities or areas of bone resorption. Bone scans are also useful. In these studies, a dye containing a radioactive ion is injected into the body. Areas of bone resorption have an affinity for the ion, so they will light up on the scan if the ions are absorbed. In addition, blood levels of an enzyme called alkaline phosphatase are typically elevated in people with Paget’s disease.
Bisphosphonates, drugs that decrease the activity of osteoclasts, are often used in the treatment of Paget’s disease. However, in a small percentage of cases, bisphosphonates themselves have been linked to an increased risk of fractures because the old bone that is left after bisphosphonates are administered becomes worn out and brittle. Still, most doctors feel that the benefits of bisphosphonates more than outweigh the risk; the medical professional must weigh the benefits and risks on a case-by-case basis. Bisphosphonate treatment can reduce the overall risk of deformities or fractures, which in turn reduces the risk of surgical repair and its associated risks and complications.
Blood and Nerve Supply
The spongy bone and medullary cavity receive nourishment from arteries that pass through the compact bone. The arteries enter through the nutrient foramen (plural = foramina), small openings in the diaphysis. The osteocytes in spongy bone are nourished by blood vessels of the periosteum that penetrate spongy bone and blood that circulates in the marrow cavities. As the blood passes through the marrow cavities, it is collected by veins, which then pass out of the bone through the foramina.
In addition to the blood vessels, nerves follow the same paths into the bone where they tend to concentrate in the more metabolically active regions of the bone. The nerves sense pain, and the nerves also play roles in regulating blood supplies and in bone growth, hence their concentrations in metabolically active sites of the bone.
Section Review
A hollow medullary cavity filled with yellow marrow runs the length of the diaphysis of a long bone. The walls of the diaphysis are compact bone. The epiphyses, which are wider sections at each end of a long bone, are filled with spongy bone and red marrow. The epiphyseal plate, a layer of hyaline cartilage, is replaced by osseous tissue as the organ grows in length. The medullary cavity has a delicate membranous lining called the endosteum. The outer surface of bone, except in regions covered with articular cartilage, is covered with a fibrous membrane called the periosteum. Flat bones consist of two layers of compact bone surrounding a layer of spongy bone. Bone markings depend on the function and location of bones. Articulations are places where two bones meet. Projections stick out from the surface of the bone and provide attachment points for tendons and ligaments. Holes are openings or depressions in the bones.
Bone matrix consists of collagen fibres and organic ground substance, primarily hydroxyapatite formed from calcium salts. Osteogenic cells develop into osteoblasts. Osteoblasts are cells that make new bone. They become osteocytes, the cells of mature bone, when they get trapped in the matrix. Osteoclasts engage in bone resorption. Compact bone is dense and composed of osteons, while spongy bone is less dense and made up of trabeculae. Blood vessels and nerves enter the bone through the nutrient foramina to nourish and innervate bones.
Review Questions
Critical Thinking Questions
Click the drop down below to review the terms learned from this chapter.

