Child Maltreatment
Govind Krishnamoorthy; Kay Ayre; Bronwyn Rees; and Samantha Brown
Abstract
Research across several decades has repeatedly pointed to the high prevalence of child maltreatment in our communities, and its life-long impact on our physical and mental health. This chapter will: provide an overview of key theoretical models of the nature and impact of child maltreatment; explore key principles of practice and treatment modalities when working with at-risk families; and conclude with a discussion of the need for counsellors to practice self-awareness, self-reflection, and self-care when working with such vulnerable populations.
Learning Objectives
- Identify the prevalence and aetiology of child maltreatment.
- Explore the impact of child abuse and neglect on physical and mental health.
- Identify general principles of trauma-informed care as it relates to screening, assessment, and intervention.
- Identify common interventions and programs utilised with children and families where there are concerns of child maltreatment.
- Evaluate the impact of traumatic stress on counsellors and organisations.
Introduction
Bowlby (1977) argued that humans need to make strong emotional bonds and these bonds are initially with their caregivers. What happens when this is disrupted and becomes unsafe? What can we, as counsellors, do to support children and families in situations where their fundamental needs aren’t being met?
Research across several decades has exposed a high prevalence of child maltreatment in communities around the world, and shone new light on the far-reaching impact on health and wellbeing across the lifespan. Adversity and maltreatment in childhood may be the result of intentional or unintentional caregiving behaviours, and can include acts of omission (e.g., neglecting to provide sufficient food or shelter) and commission (e.g., physical abuse in the form of excessive physical discipline) (Bromfield et al., 2007). Fraught with heart-breaking situations that are complex and multilayered, working in the area of child maltreatment requires counsellors to not only be aware of best practice standards, but also reflective of their own reactions and wellbeing. Furthermore, given the high prevalence and deleterious impact of child maltreatment, all counsellors irrespective of their chosen area of practice, have a responsibility to be familiar with the complex nature of child maltreatment and how to best support these vulnerable families.
How are child abuse and neglect defined?
In the early 1960s, Dr. C. Henry Kempe and his associates identified the ‘battered child syndrome’ after encountering a number of children presenting to hospital with unexplained fractures and subdural hematomas, and speculated that they may have been inflicted by the parents (Kempe et al., 1962). The published findings described the scope of child abuse, and the report shocked many medical and social service professionals. The identification of this phenomenon drew significant attention to the problem. Since this time, definitions of various forms of child maltreatment have changed and have been debated around the world. Child maltreatment includes physical maltreatment, emotional maltreatment, sexual abuse, and/or neglect. These forms result in actual or potential harm to the child including to their health, development, dignity, and in extreme cases, survival (Butchart et al., 2006).
There are several forms of child maltreatment. The physical abuse of a child is defined as those acts of commission by a caregiver that cause actual physical harm or have the potential for harm (Mikton & Butchart, 2009). Sexual abuse is defined as those acts where caregivers use a child for sexual gratification (WHO, 2006). Definitions of emotional abuse include the failure of a caregiver to provide an appropriate and supportive environment, and include acts that have adverse effects on the emotional health and development of a child (WHO, 2006). Such acts include restricting a child’s movements, denigration, ridicule, threats and intimidation, discrimination, rejection, and other non-physical forms of hostile treatment. Neglect refers to the failure of a caregiver to provide for the development of the child – where the caregiver is in a position to do so – in one or more of the following areas: health, education, emotional development, nutrition, shelter, and safe living conditions (WHO, 2006). Neglect is thus distinguished from circumstances of poverty in that neglect can occur only in cases where reasonable resources are available to the family and caregiver. Emerging research has also pointed to the adverse impact of witnessing domestic and family violence on children, with several scholars suggesting it as a form of child maltreatment in and of itself (Bromfield et al., 2007). The research literature demonstrates that witnessing can involve a much broader range of incidents, including the child hearing the violence; being used as a physical weapon; being forced to watch or participate in assaults, or being informed that they are to blame for the violence because of their behaviour (Humphreys, 2007). Children’s exposure to domestic and family violence has been found to have both short-term and long-term impacts on their development. Indeed, several studies indicate that the relation between exposure to violence and child adjustment problems is evident for periods of 10 years or more (e.g., Narayan et al., 2013).
Epidemiology: The extent of the problem
While child maltreatment was previously believed to be a rare or infrequent occurrence, large-scale epidemiological studies have discovered higher rates of child maltreatment in the general population. The Adverse Childhood Experiences (ACE) Study (Felitti, 1998) in the United States found that up to two thirds of the adults surveyed in the study reported the experience of one or more types of adverse childhood events, and up to 87% of the sample reported the experience of two or more types of such events (Anda et al., 2006). Prevalence estimates ranged from 5%-18%, with the majority of studies finding rates between 5% and 10%. Three contemporary Australian studies have measured child neglect in community samples (Price-Robertson et al., 2010). Prevalence estimates of neglect ranged from 1.6% to 4%. Three recent Australian studies and one Australian systematic review have estimated the prevalence of emotional maltreatment. Although the studies were all conducted with relatively large community samples, their prevalence estimates were quite different, ranging from 6% (Rosenman & Rodgers, 2004) to 17% (Price-Robertson et al., 2010). The best available evidence suggests that the prevalence rate for emotional maltreatment in Australia is between 9% and 14% (Chu et al., 2013; Moore et al., 2015). Community-based studies have estimated the extent to which Australian children are exposed to family violence – ranging from 4% to 23% of children (Price-Robertson et al., 2010).
Theories of child maltreatment
The first major movement to protect children began during the early 1800s the doctrine of parens patriae (literally, the “state as the father”) was introduced into English law to protect the rights of children. It allowed children to “emancipate” into adulthood at age 21 and protected the property rights of minors when the caregiver was abusing these rights. Since this time, many theories have been used to explain child maltreatment. The historical evolution of theories about child maltreatment falls into four progressive stages. The first is the “speculation” period of the 1960s when the phenomenon of child abuse and neglect first came into public awareness. The second is the “introspection” period of the 1970s when unidimensionality theories were prevalent. Third is the “diversity” period that explored more ecologically based theoretical explanations. Fourth was the 1990s classified as “multidisciplinary integration” with the embrace of the ecological-transactional model of child maltreatment that guides much of maltreatment practice and research today.
Bronfenbrenner (1979) first proposed an ecological perspective of human development, and Belsky (1980) applied the model to child maltreatment. What separates the ecological model from other theoretical models is its deviation from single-focused processes to a transactional and multilevel explanation. Belsky (1980) coupled the theoretical models of Bronfenbrenner and Tinbergen to develop the ecological model. It is explained in four levels: (1) ontogenic; (2) microsystem; (3) exosystem; and (4) macrosystem (See Figure 1). Ontogenic factors relate to the childhood histories of abusive caregivers (Belsky, 1980). The purpose of this exploration is to assess how a particular caregiver grows to behave in an abusive manner. The occurrence of abuse or neglect in childhood alone is insufficient to explain the phenomenon of child maltreatment because the majority of those who were maltreated fail to maltreat their own children. Yet the developmental history of the caregivers may predispose them to respond to certain situations in the microsystem or exosystem. The microsystem refers to the immediate context in which child maltreatment takes place and includes the family system, the maltreatment itself, and both caregiver and child characteristics. The exosystem encompasses the individual and family within larger social structures, including both formal and informal structures.
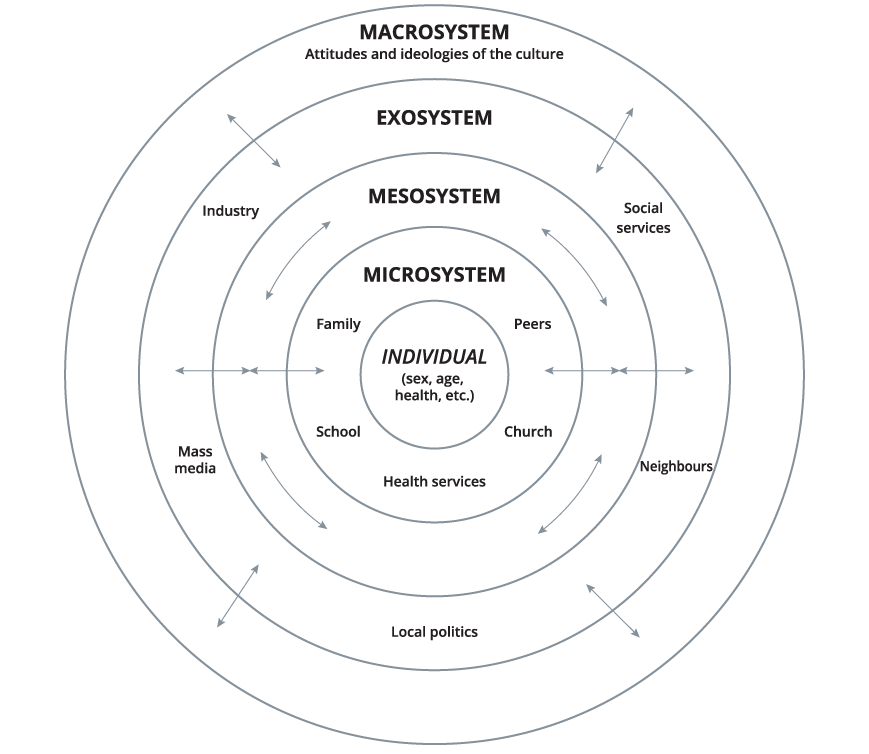
More recently, researchers have focused on the cumulative risk hypothesis that posits that human development may be jeopardized by “constellations of risk” rather than isolated adverse events (see Figure 1; Evans et al., 2013). Referred to as the cumulative ecological transactional models of child maltreatment, such models suggest that the psychological health outcomes of children are dependent on the accumulation of risk factors across contexts (e.g., home, school) and time (e.g., during infancy, early childhood, adolescence) (Bryce, 2018). Measures of the effects of such cumulative harm have been found to be predictive of a wide range of physical and mental health problems, such as paediatric asthma (Everhart et al., 2008), obesity (Evans et al., 2013), stroke (Mohan et al., 2011), and psychiatric disorders (Gruhn & Compas, 2020). These risk and protective factors are discussed further in the next section.
Learning activity 1
Listen to Professor Cicchetti speak about Child Maltreatment [47:42].
Aetiology: What are the risk factors for child abuse and neglect?
As discussed in the earlier section, there is no single factor which causes child abuse and neglect. Factors related to the characteristics of the child that increase the risk of maltreatment include the age, sex, and presence of a disability. Fatal cases of physical abuse are found largely among young infants (Berkowitz, 2017). Physical abuse seems to peak for children at the age of 6 to 12 years (Fingarson et al., 2019). Sexual abuse rates, on the other hand, tend to rise after the onset of puberty, with the highest rates occurring during adolescence (Fingarson et al., 2019). In most countries around the world, girls are at higher risk than boys for infanticide, sexual abuse, educational and nutritional neglect, and forced prostitution. Male children have been identified as being at greater risk of harsh physical punishment (Berkowitz, 2017). Premature infants, twins, and children with disabilities have been shown to be at increased risk for physical abuse and neglect (Henry, 2020).
The multiple determinants of child maltreatment have important implications for how counsellors understand a child and family’s needs and how they plan their interventions. Lay explanations of why child maltreatment occurs may be overly simplistic, (e.g., blaming caregivers for not taking sufficient responsibility, or blaming societal trends and incidences on the increased incidence). Assessment of a child and a family’s needs across multiple domains and systems may highlight to the counsellor the systemic needs of both the child and the family that may need to be addressed, either before or in conjunction with, the counselling provided to the family.
The impact of child abuse and neglect: Biopsychosocial effects
Children are impacted by maltreatment in various ways. Bromfield et al. (2007) describe key dimensions by which children may vary in their experience of abuse and neglect:
- the types of abuse and neglect the child is exposed to (e.g., sexual abuse, physical abuse, neglect)
- the frequency, severity, and duration of the maltreatment
- the age and developmental status of the child when the abuse occurred
- the relationship between the child and those who are seen as linked to the maltreatment occurring.
Child abuse and neglect that occurred over different development stages has been found to have a profound and exponential impact over a child’s life, with adverse consequences felt throughout the life course (Masten, 2018). Such findings highlight the importance of considering the history of maltreatment and its impact on the individual, rather than just an isolated episode of abuse. Referred to as ‘multitype maltreatment’, vulnerable children are most often exposed to a number of different forms of maltreatment experiences across their development (Higgins & McCabe, 2003). This is an important consideration to understand the cumulative harm experienced by children, and their ongoing cumulative and chronic risk into the future (Sheehan, 2019).
Neurobiological development
Infancy and early childhood are marked by rapid growth of the brain. Between birth and two years of age, the number of neurons, the cells that make up the brain, are said to have increased by 500% (McCrory et al., 2017). This rapid development of the brain is dependent on the child’s early experiences and the environments they live in. Thus, appropriate and responsive care and stimulation are important in order to allow for optimal growth of brain circuitry (Sheridan & Nelson, 2009). Researchers studying young children who were deprived of appropriate care have found significant decreases in overall brain size and volume (Perry, 2008). A decrease was particularly noted in children’s prefrontal cortex, often associated with complex cognitive tasks, such as decision making and controlling emotions (McCrory et al., 2017; Perry, 2008). Research on the physiological effects of maltreatment have focused on changes to the human stress response – a complex phenomenon involving multiple human organs, designed to help us respond to threats and danger in our environment (LeDoux & Pine, 2016). This stress response is said to have evolved as a survival mechanism, enabling people and other mammals to fight the threat off or flee to safety. Unfortunately, chronic exposure to stressful experiences may mean that our bodies overreact to stressors that are not life-threatening, such as traffic jams, work pressure, and family difficulties (LeDoux & Pine, 2016). Findings have consistently shown that prolonged and chronic exposure to stress, sometimes referred to as ‘toxic stress’, alters the function and pattern of the physiological stress systems in children. This causes the child to either react with excessive feelings of stress to potentially benign situations and/or to not identify or act protectively in situations of potential danger and threat (Cicchetti et al., 2011).
Resource: For an introduction to the impact of child maltreatment on the brain, be sure to read Dr. Bruce Perry’s seminal book, ‘The Boy Who Was Raised as a Dog: What traumatised children can teach us about loss, love and healing’.
Cognitive and language development
Research has repeatedly found that exposure to adverse experiences early in childhood is consistently associated with critical lags in cognitive development and numerous academic difficulties (Chugani et al., 2001; Gould et al., 2012) associated with attention, language skills and working memory. Cognitive and language competencies are strong indicators of a child’s school readiness with respect to literacy, capacity to follow instructions, receptivity to performance evaluations, and ability to navigate peer interactions (Spratt et al., 2012). As early childhood is a sensitive period for language development, maltreated children are at particular risk for language delays. In a meta-analytic review examining maltreatment and language, Sylvestre et al. (2016) found that the language skills of children who have experienced abuse or neglect are delayed when compared to children without such experience with young children being particularly vulnerable to the language effects of maltreatment.
Social and emotional development
Social and emotional development involves the capacity to understand the self and others, to form relationships and to experience, regulate and express emotions. The development of such skills depends on the quality of relationships and the childhood caregiving environment (Thompson, 2016). Attachment theory, first formulated by the psychoanalyst John Bowlby, emphasised the need for infants to have an attachment to their caregivers. This attachment is a strong emotional bond, where caregivers were perceived as a source of comfort and reassurance, rather than just a source of fear and harm (Bowlby, 1977). Bowlby hypothesised that attachment relationships had evolved to maintain proximity between infants and their caregivers, to increase the chance of protection – particularly in times of danger and threat.
Building on Bowlby’s work, and utilising observations of separations and reunions among infants and their caregivers, Mary Ainsworth identified three distinct patterns of infant attachment or attachment styles. The three styles were secure, anxious-resistant and avoidant. Children classified as secure attached were found to welcome their caregiver’s return after separations, and if distressed, sought proximity and comfort from them (Ainsworth et al., 1978). In contrast, infants classified as having ‘insecure attachments’ were found to either follow an anxious-resistant or anxious-avoidant pattern. Anxious-resistant infants were found to show ambivalent behaviours towards their caregiver and an inability to be comforted during reunions with their caregivers. Infants classified as anxious-avoidant were found to avoid proximity or interaction with the caretaker on reunion (Ainsworth et al., 1978). More recent research has pointed to the presence of a fourth attachment style, commonly observed in maltreated children, labelled as ‘disorganised’. It is a mix of anxious-ambivalent and anxious-avoidant attachment styles – frequently observed amongst infant and children exposed to unpredictable, chaotic, and frightening caregiving relationships and environments (Main & Solomon, 1990). Population level studies on attachment styles have found that up to 55-59% of children have secure attachment styles, avoidant attachment styles constitute up to 25% and anxious attachment in 11 to 20% of the population. The disorganised attachment styles have been found to be prevalent in the general population between 1 to 5%, with up to 85% of children in foster care displaying behaviours consistent with a disorganised attachment style (Mickelson et al., 1997).
Learning activity 2
For an illustration of the importance of healthy childhood attachment, watch this video of Professor Edward Tronick’s landmark research utilising the ‘still face’ paradigm [2:49].
Children’s mental health
The impact of maltreatment on mental health has primarily been studied through its manifestations in symptoms of post-traumatic stress disorder (PTSD). Childhood trauma, and the resultant ‘toxic stress’ response, has been defined as the emotional reaction to exposure to an event that threatens or causes harm to a child’s emotional and physical wellbeing (NCTSN, 2015). PTSD symptoms can manifest themselves in the form of: re-experiencing the traumatic event (often through play in children); avoidance of triggers that serve as reminders of the frightening and traumatic experience; hyper-arousal; disturbed sleep; increased irritability, aggression, and alertness; temper tantrums; and startled and extreme responses to stimuli (Scheeringa et al., 2015). Individuals with a history of childhood maltreatment were found to have poor response to treatment compared to non-maltreated individuals with similar mental health diagnoses (Teicher & Samson, 2016).
Screening and assessment
The first step in helping children who have been maltreated is to recognise signs of maltreatment as part of the screening and assessment process. The presence of a single sign does not necessarily mean that child maltreatment is occurring in a family, but a closer look at the situation may be warranted when these signs appear repeatedly or in combination. The assessment of the presence and impact of child maltreatment is crucial as part of a rigorous screening and assessment process. For children and adolescents, identifying the signs of maltreatment and acting protectively addresses immediate safety concerns and stops the continuing victimisation of the child or adolescent.
A child may directly disclose to you that he or she has experienced abuse or neglect. In such cases, it is important that you are acquainted with the relevant child protection legislative requirements of the jurisdiction in which you are working, and be aware of your organisation’s child reporting requirements. In Queensland, Australia, the Child Protection Act 1999 (Qld) requires certain professionals, referred to as ‘mandatory reporters’, to make a report to child protection services, if they form a reasonable suspicion that a child has suffered, is suffering, or is at an unacceptable risk of suffering significant harm caused abuse, and may not have a caregiver able and willing to protect them. Please note that counsellors may or may not be considered mandatory reporters – depending on your occupational setting and state or territory level legislation. As requirements are different across states in Australia, and across services, it is advised that you seek clarifications regarding your role in reporting child protection concerns.
Learning activity 3
Making decisions about removing a child from a potentially unsafe home environment can be complex. The Australian Broadcasting Corporation (ABC) offer an interactive news article to illustrate the complexities of decisions in child protection: You decide: Would you remove these children from their families?
Prior to assessing the impact of child maltreatment, it is worth considering your role in the service within which you work, and how you may explain your role to the children and families with whom you are working. For example, some young clients might assume that counsellors are the police or child protective services and that they may get into trouble or removed for making disclosures or discussions of the impact of traumatic experiences. The process of assessment can require more than a single session to complete and should also use multiple avenues to obtain the necessary clinical information, including self-assessment tools (see Resource section below), past and present clinical and medical records, structured clinical interviews, assessment measures, and collateral information from significant others, other behavioural health and child protection professionals and agencies.
Learning activity 4
There are a number of psychometric assessment tools that can support your assessment and monitoring of trauma symptoms in children and adolescents. The National Child Traumatic Stress Network (NCTSN) from the United States offers a contemporary review of a number of reliable and valid measures: All measure reviews
Practice implications
The following are some considerations when conducting assessments with clients exposed to child maltreatment.
Clarify for the client what to expect in the screening and assessment process
Inform the client, in a developmentally appropriate manner, that the screening and assessment phase focuses on identifying issues that might benefit from treatment. Inform them that during the interview, uncomfortable thoughts and feelings can arise. Provide reassurance that, if they do, you will assist in dealing with this distress, but also let them know that, even with your assistance, some psychological and physical reactions to the interview may last for a few hours or perhaps as long as a few days after the interview, and be sure to highlight the fact that such reactions are normal (Read et al., 2003).
Approach the client in a matter-of-fact yet supportive manner
Such an approach helps create an atmosphere of trust, respect, acceptance, and thoughtfulness (Melnick & Bassuk, 2000). Doing so helps to normalise symptoms and experiences generated by the maltreatment; consider informing clients that such events are common but can cause continued emotional distress if they are not treated. Clients may also find it helpful for you to explain the purpose of certain difficult questions. Demonstrate kindness and directness in equal measure when assessing clients (Najavits, 2002).
Respect the client’s personal space
Cultural and ethnic factors vary greatly regarding the appropriate physical distance to maintain during the interview. You should respect the client’s personal space, sitting neither too far from nor too close to the client. Let your observations of the client’s comfort level during the screening and assessment process guide the amount distance and position in the room. Clients with trauma may have particular sensitivity about their bodies, personal space, and boundaries.
Adjust tone and volume of speech to suit the client’s level of engagement and degree of comfort in the interview process
Strive to maintain a calm and quiet demeanour. Be sensitive to how the client might hear what you have to say in response to personal disclosures. Clients who have been experiencing symptoms of trauma may be more reactive even to benign or well-intended questions. Avoid phrases that imply judgement about the maltreatment. For example, questions such as “why didn’t you tell someone when it happened?” may imply blame and not sufficiently acknowledge complex psychological processes linked to shame, shock and stigma related to experiences of abuse and neglect.
Provide appropriate symbols of safety in the physical environment
These include paintings, posters and other room decorations that symbolise the safety of the surroundings to the client population. Such considerations may be particularly pertinent for children with autism and developmental disabilities, who may experience sensory issues. This can involve both hyper-sensitivities (over-responsiveness) and hypo-sensitivities (under-responsiveness) to a wide range of stimuli, including particular lights, sounds, and smells in the counselling setting. An assessment of such sensory sensitivities and preferences with such children may be advised.
Give the client as much personal control as possible during the assessment
Present a rationale for the interview and its stress-inducing potential, making clear that the client has the right to refuse to answer any and all questions. Giving the client (where staffing permits) the option of being interviewed by someone of the gender with whom he or she is most comfortable, postponing the interview if necessary (Harris & Fallot, 2001).
Allow time for clients to become calm and oriented to the present if they experienced very intense emotional responses when recalling or acknowledging feelings of distress
At such times, avoid responding in excessively emotive ways (Bernstein, 2000). If the client has difficulty self-soothing, guide them through strategies to help them with their distress (e.g., grounding exercises).
Be mindful of barriers to disclosing child maltreatment
There are two main barriers to the evaluation of child maltreatment and its impact on clients. The first is related to differences in the perceptions between the client and the counsellor in regard to what is considered abuse and neglect. Some clients might not have ever thought of a particular event as abusive, or their response to it as traumatic, and thus might not report or even recall the event. Some clients might feel a reluctance to discuss something that they sense might bring up uncomfortable feelings (especially with a counsellor whom they have only recently met). Clients may avoid openly discussing traumatic events or have difficulty recognising or articulating their experience of trauma for other reasons, including a feeling unsafe to share experiences, feelings of shame, guilt, or fear of retribution by others associated with the event (e.g., in cases of interpersonal or domestic violence). Still others may deny their history because they are tired of being interviewed or asked to fill out forms and may believe it does not matter anyway.
Cultural considerations
Finally, as with all other presenting concerns, the screening and assessments of child maltreatment must take adequate consideration of culture, ethnicity, and race. Factors, such as norms for expressing psychological distress and the stigma associated with seeking help may influence engagement with the assessment process.
Intervention: Trauma-informed care and specific intervention modalities
Trauma-informed care
With increasing recognition of the pervasiveness of child abuse and neglect, and the impact of traumatic stress on children and families, awareness is growing of the importance of ‘trauma-informed’ approaches to psychological interventions. Trauma-informed care refers to the understanding, anticipating, and responding to issues, expectations, and special needs that a person who has been victimised may have in a particular setting (Lang et al., 2016). At a minimum, trauma-informed practitioners must endeavour to do no harm—that is, to avoid re-traumatising or blaming clients for their efforts to manage their traumatic reactions (Fallot & Harris, 2008). Trauma-informed care requires a commitment from practitioners and services to understanding traumatic stress and to developing strategies for responding to the complex needs of survivors.
Practice implications: Trauma-informed care principles
Harris and Fallot (2001) have summarised trauma-informed care as being grounded in eight key principles. These are:
1. Understanding trauma and its impact
Understanding traumatic stress and how it impacts people and recognising that many behaviours and responses that may seem ineffective and unhealthy in the present, represent adaptive responses to past traumatic experiences.
2. Promoting safety
Establishing a safe physical and emotional environment where basic needs are met, safety measures are in place, and provider responses are consistent, predictable, and respectful.
3. Ensuring cultural competence
Understanding how cultural context influences one’s perception of and response to traumatic events and the recovery process; respecting diversity, providing opportunities for clients to engage in cultural rituals, and using interventions respectful of and specific to cultural backgrounds.
4. Supporting control, choice, and autonomy
Helping clients regain a sense of control over their daily lives and build competencies that will strengthen their sense of autonomy; keeping consumers well-informed about all aspects of the system, outlining clear expectations, providing opportunities for clients to make daily decisions and participate in the creation of personal goals, and maintaining awareness and respect for basic human rights and freedoms.
5. Sharing power and responsibility
Promoting democracy and equalisation of the power differentials across the program; and sharing power and decision-making across all levels of an organization, whether related to daily decisions or in the review and creation of policies and procedures.
6. Integrating care
Maintaining a holistic view of consumers and their process of healing and facilitating communication within and among service providers and systems.
7. Healing happens in relationships
Believing that establishing safe, authentic, and positive relationships can be corrective and restorative to survivors of trauma.
8. Recovery is possible
Understanding that recovery is possible for everyone regardless of how vulnerable they may appear; instilling hope by providing opportunities for consumer and former consumer involvement at all levels of the system, facilitating peer support, focusing on strength and resiliency, and establishing future-oriented goals.
In this way, trauma-informed care is grounded in an understanding of and responsiveness to the impact of trauma. Such practices emphasise the physical, psychological, and emotional safety for both providers and survivors, and that creates opportunities for survivors to rebuild a sense of control and empowerment. Given the prevalence of childhood adversity, and the complex nature of assessing for these concerns, the principles of trauma-informed care form a standard for how interventions and practices are delivered to all clients – not simply those who are diagnosed with PTSD, or have disclosed being exposed to traumatic experiences.
Prevention and intervention
Counsellors have an important role to play in designing and implementing primary prevention programmes for child maltreatment. At present, there are relatively few evidence-based interventions available for children exposed to child maltreatment, and their families (Altafim & Linhares, 2016). Research on efficacious interventions following concerns of child abuse and neglect involves a multi-systemic approach – with a focus on interventions targeted at both the child and significant adults in the child’s life. While it is beyond the scope of this chapter to provide a detailed of interventions in detail, the remainder of this section will briefly review some promising approaches and programs for children of various ages.
Children under five years
For young children, attachment-based interventions focused on improving the relationships between children and their key attachment figures (often, caregiver) are recommended. Programs such as the attachment and biobehavioural catch-up (Dozier et al., 2017) help the caregiver to respond more sensitively to children. Another example of such promising intervention is the circle of security parenting program (Cooper et al., 2009). The program focuses on attachment. COSP takes an innovative approach to help caregivers increase their capacities to serve as a source of security for their children (i.e., to provide a secure base) (Bowlby, 1988), with the idea that this increases caregiver sensitivity and reduces the risk of insecure and disorganised attachment. This intervention was designed with implementation efficiencies and value in mind, in collaboration with staff from the real-world contexts in which it is to be implemented and the diverse at-risk families it is intended to serve (e.g., early childhood programs) (Cooper et al., 2009). Similarly, the program child-parent psychotherapy (CPP) (Lieberman et al., 2006) uses the attachment relationship as the vehicle for improving the child’s emotional, cognitive, and social functioning. The child and caregiver are seen in joint sessions that focus on promoting emotion regulation in both the child and the caregiver (Lieberman et al., 2006).
Children aged 12 and under
Significant research has focused on interventions aimed at improving parenting/caregiving skills amongst families using principles of behavioural theory and operant conditioning (Skinner, 1972). For example, Pathways’ triple P (Petra & Kohl, 2010), a modified version of the evidence-based parenting program triple P (Sanders et al., 2003), has shown promise in improving parenting/caregiving skills and attitudes, increasing parenting/caregiving efficacy, and reducing child behaviour problems of at-risk children and families (Sanders et al., 2004). Certain interventions have aimed to help parents/caregivers with other psychological problems which are not exclusively associated with the parenting/caregiving role, such as anger management, mood regulation, and addressing drug abuse. For example, the parenting under pressure (PUP) program (Harnett & Dawe, 2008) is an intensive, home-based intervention underpinned by two key constructs: (i) that child wellbeing is dependent on the parent/caregiver’s capacity to provide a sensitive, responsive and nurturing caregiving environment; and (ii) that in order for this to occur, a parent/caregiver needs to be able to understand and manage their own affect both in relation to parenting/caregiving and to managing substance abuse problems (Barlow et al., 2013).
The emergence of neuroscientific impacts of child maltreatment on the brain has spurred the development of programs such as the neurosequential model of therapeutics (NMT) (Perry, 2006). NMT offers assessments to children exposed to maltreatment and other forms of trauma, to support the sequencing of interventions (educational, enrichment, and therapeutic) in a way that reflects the child’s specific developmental needs in a variety of key domains, and is sensitive to core principles of neurodevelopment (Perry, 2008). With older children, the negative self-evaluative beliefs and beliefs about power and violence in relationships that evolve in response to the experience of abuse may be addressed in individual therapy (e.g., trauma focused cognitive behaviour therapy (TF-CBT) (Cohen et al., 2012), or even group therapy (e.g., dialectical behaviour therapy for adolescents (DBT-A) (Rathus & Miller, 2014).
Children and young people aged 17 and under
Interventions for older adolescents have focused on the wider system and aim to reduce stress and increase social support. Programs such as the multisystem therapy for child abuse and neglect (MST-CAN) (Swenson & Schaeffer, 2014) offer interventions that are tailored to the ecology of the family as mapped out during the assessment process. Some examples of interventions are working with the extended family to increase the amount of support they offer the child’s primary caretaker; arranging a befriender, a home help or a counsellor home-visiting service for an isolated parent; arranging participation in a local parent support self-help group; or organising a place for the child and caretaker in a local mother and toddler group (Swenson & Schaeffer, 2014). In this way, the program acknowledges the factors across various systems impacting a child and their family, and works to modify aspects of these environments to mitigate the risks of child maltreatment in the future.
Professional issues: Secondary traumatic stress and self-care
Learning about child maltreatment often invokes strong feelings among health professionals. For example, some counsellors develop a strong urge to protect the child at all costs – minimising or denying any loyalty the child may have towards their caregivers, or any potential for change on the part of the caregivers. Another common reaction can be a strong urge to protect or rescue the caregivers. In these cases, the counsellor may defend criticisms raised about the caregivers by other professionals, explain away or deny any caregiving shortcomings. These reactions may get in the way of professionals cooperating with each other and working in the best interests of the family. For example, many counsellors have had some personal loss or even traumatic experience in their own life (e.g., loss of a family member, death of a close friend). To some extent, the pain of experiences can be “re-activated.” Therefore, when professionals work with an individual who has suffered similar trauma, the experience often triggers painful reminders of their own trauma. Developing self-awareness of such reactions and finding ways of being reflective of our work and thoughtful in our interactions, are important for working in cases involving child maltreatment. The following section will briefly describe common reactions to working with child maltreatment and childhood trauma. Strategies to manage one’s own reactions will be reviewed, and practical strategies for self-care to prevent burnout among counsellors.
Secondary traumatic stress and counsellors
Secondary traumatic stress is a risk we incur when we engage empathically with an adult or child who has been traumatised. Secondary traumatic stress is commonly defined as a set of natural, consequent behaviours resulting from knowledge about a traumatising event experienced by a significant other (Figley, 1995). It is the stress resulting from wanting to help a traumatised or suffering person. It has only been recently that researchers and practitioners have acknowledged that professionals who work with or help people with childhood maltreatment or trauma are indirectly or secondarily at risk of developing the same symptoms as persons directly affected by the traumatic events. Counsellors who listen to adults or children describe the trauma are at risk of absorbing a portion of the trauma (Carr, 2015).
Practice implications: Self-care for individuals; Prevention and management
Training, support, and professional supervision can all reduce the risk of counsellors developing secondary traumatic stress disorder. Understanding what secondary trauma is and what causes it reduces a person’s vulnerability and increases resilience. Training in managing stress will increase a counsellor’s ability to respond to stress in ways that are less damaging. Similarly, training aimed at personal development also increases the counsellor’s sense of having an identity outside of work. Improving skills in a sport, or some other pursuit such as music or dance, increases the sense of joy in living which helps to protect us from the effects of stress (Brady, 2012). An audit of one’s social support network, and methods to increase the quality of the support one is receiving, is possibly the most useful exercise in self-care. Informal support may come from people within the individual’s network who are familiar with the concept of secondary traumatic stress disorder and who recognise the signs. Regular de-briefing or feedback session that looks for any changes that might indicate that the person is developing a secondary stress disorder is critical for good self-care (Salloum et al., 2015). For counsellors in Australia, professional development and involvement with counselling associations, such as Psychotherapy and Counselling Federation of Australia (PACFA) or Australian Counselling Association (ACA), offer counsellors opportunities to network with other counsellors, seek peer support, and participate in group supervision.
Secondary traumatic stress and organisations
It is important to note here that self-care is not solely the responsibility of the counsellors themselves. In fact, without sufficient recognition or support from service, teams, or organisations, many of the self-care strategies fall short of protecting counsellors from burnout. Social services and counselling organisations working in the child welfare sector often find themselves operating in the face of recurrent or constant crises. When left unchecked, such chronic stress has been found to influence organisational culture, leading to staff being unable to constructively confront problems, engage in complex problem-solving, and be involved in all levels of staff decision making processes (Bloom, 2008). In her seminal work on the impact of traumatic stress on organisations, Sandra Bloom (Bloom & Farragher, 2013) describes ‘parallel processes’ within organisations, where communication networks tend to break down under stress, much like they do within vulnerable families that are the clients of the services. When communication networks break down in these services, so too do the feedback loops that are necessary for consistent and timely error correction (Bloom, 2008). As decision-making becomes increasingly non-participatory and problem-solving more reactive, an increasing number of short-sighted policy decisions are made that appear to compound existing problems. Fallot and Harris (2008) describe a process by which organisations can start by looking at shared assumptions, goals, and existing practices with staff from various levels of the organisation. Trauma-informed processes have been found to improve staff morale, as the leadership is seen as being open to new sources of information. Such organisational practices emphasise the development of more democratic, participatory processes is critical as these are the processes most likely to lend themselves to promoting self-awareness amongst staff, and support in the development of solutions to the often complex problems facing the organisation (Bloom, 2008).
Learning activity 5
Learn more about the impact of traumatic stress on organisations in our interview with Dr. Sandra Bloom on the trauma-informed education podcast.
Conclusion
Child maltreatment is a complex and multifactorial phenomenon. This chapter provides a cursory overview of some of the key considerations for counsellors in their work with children and their families. Counsellors are encouraged to be mindful of key risk factors associated with child maltreatment, and the cumulative impact of these problems and challenges faced by children and their families. From assessment to ongoing counselling, the provision of trauma-informed care is characterised by practices that ensure the physical and psychological safety of children and their families. By collaborating effectively with families and key stakeholders, counsellors can support children in their recovery from child abuse and neglect. The sustainable provision of support requires practitioners to attend to their own wellbeing, while being equally supported by the organisations that employ them. Despite the devastating impact of child maltreatment, the presence of a calm, caring and reflective adult is often the key ingredient to a child’s journey of healing from a traumatic past.
Learning activity 6
Watch this video of a clinician conducting an interview to assess for concerns of maltreatment [16:19]. Despite being an instructional video, there are aspects of the interview that could be done different.
As you watch the video, consider the following questions:
What do you think of the physical environment in which the session is being conducted? How do you think it helps and in what way might it hinder the session?
What do you think of the language used and the communication style? Are there similarities or differences to how you may phrase questions and statements?
In what way might the interview be more “trauma-informed”?
Learning activity 7
Watch this video of the interview being conducted with the child [11:41]. As you are watching, consider the questions listed in learning activity 6. Consider how the interview with the adult is different to that of the child.
Glossary of terms
aetiology—the cause, set of causes, or manner of causation of a disease and/or other factors relating to health
attachment—a strong emotional bond that an infant forms with a caregiver (such as a mother) especially when viewed as a basis for normal emotional and social development
burnout—a syndrome conceptualised as resulting from chronic workplace stress that has not been successfully managed
caregiver—an adult who is responsible for the care of a child, including parent, step-parent, adult sibling, grandparent, other family or kin member, or other appointed adult
child maltreatment—all forms of physical and/or emotional ill-treatment, sexual abuse, neglect, or negligent treatment or commercial or other exploitation, results in actual or potential harm to the child’s health, survival, development, or dignity in the context of a relationship of responsibility, trust, or power
emotional abuse—failure of a caregiver to provide an appropriate and supportive environment, and include acts that have an adverse effect on the emotional health and development of a child
exosystem—factors related to the individual and family within larger social structures, including both formal and informal structures
neglect—the failure of a caregiver to provide for the development of the child – where the caregiver is in a position to do so – in one or more of the following areas: health, education, emotional development, nutrition, shelter, and safe living conditions
microsystem—the immediate context in which child maltreatment takes place and includes the family system, the maltreatment itself, and both caregiver and child characteristics
macrosystem—factors related to the embeddedness of the individual, community, and family within the larger cultural fabric
neurobiology—the study of cells of the nervous system and the organisation of these cells into functional circuits that process information and mediate behaviour. It is a sub-discipline of both biology and neuroscience.
ontogenic factors—factors related to the childhood histories of abusive parents/caregivers
physical abuse—acts of commission by a caregiver that cause actual physical harm or have the potential for harm
post-traumatic stress disorder—a particular set of reactions that can develop in people who have been through a traumatic event which threatened their life or safety, or that of others around them
secondary traumatic stress—a set of natural, consequent behaviours resulting from knowledge about a traumatising event experienced by a significant other
self-care—the practice of taking an active role in protecting one’s own wellbeing and happiness, in particular during periods of stress
sexual abuse—acts where caregivers use a child for sexual gratification
supervision—a formal working alliance that is generally, but not necessarily, between a more experienced and a less experienced worker, in which the supervisee’s clinical work is reviewed and reflected upon with a view to improve one’s performance
trauma—reactions to the exposure to events that posed a threat to one life, or the lives of others around them
trauma-informed care—a framework for human service delivery that is based on knowledge and understanding of how trauma affects people’s lives and their service needs
References
Ainsworth, M. D., Blehar, M., Waters, E., & Wall, S. (1978). Patterns of attachment. A psychological study of the strange situation. Erlbaum.
Altafim, E. R. P., & Linhares, M. B. M. (2016). Universal violence and child maltreatment prevention programs for parents: A systematic review. Psychosocial Intervention, 25(1), 27-38.
Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Whitfield, C., Perry, B. D., Dube, S. R., & Giles, W. H. (2006). The enduring effects of abuse and related adverse experiences in childhood. European Archives of Psychiatry and Clinical Neuroscience, 256(3), 174-186. https://doi.org/10.1007/s00406-005-0624-4
Barlow, J., Sembi, S., Gardner, F., Macdonald, G., Petrou, S., Parsons, H., Harnett, P., & Dawe, S. (2013). An evaluation of the parents under pressure programme: A study protocol for an RCT into its clinical and cost effectiveness. Trials, 14(1), 210. https://trialsjournal.biomedcentral.com/articles/10.1186/1745-6215-14-210
Belsky, J. (1980). Child maltreatment: An ecological integration. American Psychologist, 35(4), 320.
Berkowitz, C. D. (2017). Physical abuse of children. New England Journal of Medicine, 376(17), 1659-1666. https://doi.org/10.1056/NEJMcp1701446
Bernstein, B. (2000). Pedagogy, symbolic control, and identity: Theory, research, critique (Vol. 5). Rowman & Littlefield.
Bloom, S. L. (2008). Understanding trauma: Integrating biological, clinical and cultural perspectives. Psychiatric Services, 59(4), 449-449.
Bloom, S. L., & Farragher, B. (2013). Restoring sanctuary: A new operating system for trauma-informed systems of care. Oxford University Press.
Bowlby, J. (1977). The making and breaking of affectional bonds: I. Aetiology and psychopathology in the light of attachment theory. The British Journal of Psychiatry, 130(3), 201-210.
Bowlby, J. (1988). Developmental psychiatry comes of age. The American Journal of Psychiatry, 145(1), 1–10. https://doi.org/10.1176/ajp.145.1.1
Brady, P. Q. (2012). Crimes against caring: Compassion fatigue, burnout and self-care practices among professionals working with crimes against children. [Masters dissertation, Boise State University]. https://scholarworks.boisestate.edu/cgi/viewcontent.cgi?article=1001&context=crimjust_gradproj
Bromfield, L. M., Gillingham, P., & Higgins, D. J. (2007). Cumulative harm and chronic child maltreatment. Developing Practice: The Child Youth and Family Work Journal, 19, 34-42.
Bronfenbrenner, U. (1979). Contexts of child rearing: Problems and prospects. American Psychologist, 34(10), 844.
Bryce, I. I. (2018) Cumulative risk and harm: The condition of accumulation in child maltreatment. Communities, Children and Families Australia, 12 (1), 7-22.
Butchart, A., Harvey, A. P., Mian, M., & Fürniss, T. (2006). Preventing child maltreatment. A guide to taking action and generating evidence. World Health Organization. https://apps.who.int/iris/handle/10665/43499
Carr, A. (2015). The handbook of child and adolescent clinical psychology: A contextual approach. Routledge.
Child Protection Act 1977 (Qld). https://www.legislation.qld.gov.au/view/html/inforce/current/act-1999-010
Chu, D. A., Williams, L. M., Harris, A. W., Bryant, R. A., & Gatt, J. M. (2013). Early life trauma predicts self-reported levels of depressive and anxiety symptoms in nonclinical community adults: relative contributions of early life stressor types and adult trauma exposure. Journal of Psychiatric Research, 47(1), 23-32.
Chugani, H. T., Behen, M. E., Muzik, O., Juhász, C., Nagy, F., & Chugani, D. C. (2001). Local brain functional activity following early deprivation: A study of postinstitutionalized Romanian orphans. Neuroimage, 14(6), 1290-1301.
Cicchetti, D., Rogosch, F. A., Toth, S. L., & Sturge-Apple, M. L. (2011). Normalizing the development of cortisol regulation in maltreated infants through preventive interventions. Development and Psychopathology, 23(3), 789-800.
Cohen, J. A., Mannarino, A. P., Kliethermes, M., & Murray, L. A. (2012). Trauma-focused CBT for youth with complex trauma. Child abuse & neglect, 36(6), 528-541.
Cooper, G., Hoffman, K. T., & Powell, B. (2009). Circle of Security: COS-P facilitator DVD manual 5.0. Marycliff Institute.
Dozier, M., Bernard, K., & Roben, C. K. (2017). Attachment and biobehavioral catch-up. In H. Steele & M. Steele (Eds.), The handbook of attachment-based interventions (pp. 27-49). The Guildford Press.
Evans, G. W., Li, D., & Whipple, S. S. (2013). Cumulative risk and child development. Psychological Bulletin, 139(6), 1342.
Everhart, R. S., Fiese, B. H., & Smyth, J. M. (2008). A cumulative risk model predicting caregiver quality of life in pediatric asthma. Journal of Pediatric Psychology, 33(8), 809-818.
Fallot, R. D., & Harris, M. (2008). Trauma-informed approaches to systems of care. Trauma Psychology Newsletter, 3(1), 6-7.
Felitti, V. J. (1998). The relationship of adult health status to childhood abuse and household dysfunction. American Journal of Preventive Medicine, 14, 245-258.
Figley, C. R. (1995). Compassion fatigue: Toward a new understanding of the costs of caring. In B. H. Stamm (Ed.), Secondary traumatic stress: Self-care issues for clinicians, researchers, and educators (pp. 3-28). The Sidran Press.
Fingarson, A. K., Pierce, M. C., Lorenz, D. J., Kaczor, K., Bennett, B., Berger, R., Currie, M., Herr, S., Hickey, S., Magana, J., Makoroff, K., Williams, M., Young, A., & Zuckerman, N. (2019). Who’s watching the children? Caregiver features associated with physical child abuse versus accidental injury. The Journal of Pediatrics, 212, 180-187. https://doi.org/10.1016/j.jpeds.2019.05.040
Gould, S. R., Beals-Erickson, S. E., & Roberts, M. C. (2012). Gaps and barriers in services for children in state mental health plans. Journal of Child and Family Studies, 21(5), 767-774.
Gruhn, M. A., & Compas, B. E. (2020). Effects of maltreatment on coping and emotion regulation in childhood and adolescence: A meta-analytic review. Child Abuse & Neglect, 103, 104446.
Harnett, P. H., & Dawe, S. (2008). Reducing child abuse potential in families identified by social services: Implications for assessment and treatment. Brief Treatment and Crisis Intervention, 8(3), 226.
Harris, M., & Fallot, R. D. (2001). Envisioning a trauma‐informed service system: A vital paradigm shift. New Directions for Mental Health Services, 89, 3-22.
Henry, B. F. (2020). Typologies of adversity in childhood & adulthood as determinants of mental health & substance use disorders of adults incarcerated in US prisons. Child Abuse & Neglect, 99, 104251.
Higgins, D. J., & McCabe, M. P. (2003). Maltreatment and family dysfunction in childhood and the subsequent adjustment of children and adults. Journal of Family Violence, 18(2), 107-120.
Humphreys, C. (2007). Domestic violence and child protection: Challenging directions for practice [Issues paper 13]. Australian Domestic & Family Violence Clearinghouse.
Kempe. C. H., Silverman, F. N., Steele, B. F., Droegemueller, W., Silver, H. K. (1962). The battered child syndrome. JAMA, 181(1), 17-24. https://doi.org/10.1001/jama.1962.03050270019004
Lang, J. M., Campbell, K., Shanley, P., Crustos, C. A., & Connell, C. M. (2016). Building capacity for trauma-informed care in the child welfare state system: Initial results of a statewide implementation. Child Maltreatment, 21(2), 113-124. https://doi.org/10.1177/1077559516635273
LeDoux, J. E., & Pine, D. S. (2016). Using neuroscience to help understand fear and anxiety: a two-system framework. American Journal of Psychiatry. https://doi.org/10.1176/appi.ajp.2016.16030353
Lieberman, A. F., Ippen, C. G., & Van Horn, P. (2006). Child-parent psychotherapy: 6-month follow-up of a randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 45(8), 913-918.
Main, M., & Solomon, J. (1990). Procedures for identifying infants as disorganized/disoriented during the Ainsworth strange situation. Attachment in the Preschool Years: Theory, Research, and Intervention, 1, 121-160.
Masten, A. S. (2018). Adult resilience after child abuse. Nature Human Behaviour, 2(4), 244-245.
McCrory, E. J., Gerin, M. I., & Viding, E. (2017). Annual research review: Childhood maltreatment, latent vulnerability and the shift to preventative psychiatry–the contribution of functional brain imaging. Journal of Child Psychology and Psychiatry, 58(4), 338-357.
Melnick, S. M., & Bassuk, E. L. (2000). Identifying and responding to domestic violence among poor & homeless women. https://nhchc.org/wp-content/uploads/2019/08/IdentifyingRespondingtoDomesticViolence_2000.pdf
Mickelson, K. D., Kessler, R. C., & Shaver, P. R. (1997). Adult attachment in a nationally representative sample. Journal of Personality and Social Psychology, 73(5), 1092.
Mikton, C., & Butchart, A. (2009). Child maltreatment prevention: A systematic review of reviews. Bulletin of the World Health Organization, 87, 353-361.
Mohan, K. M., Wolfe, C. D., Rudd, A. G., Heuschmann, P. U., Kolominsky-Rabas, P. L., & Grieve, A. P. (2011). Risk and cumulative risk of stroke recurrence: A systematic review and meta-analysis. Stroke, 42(5), 1489-1494.
Moore, S. E., Scott, J. G., Ferrari, A. J., Mills, R., Dunne, M. P., Erskine, H. E., Devries, K. M., Degenhardt, L., Vos, T., Whiteford, H. A., McCarthy, M., & Normal, R. E. (2015). Burden attributable to child maltreatment in Australia. Child Abuse & Neglect, 48, 208-220. https://doi.org/10.1016/j.chiabu.2015.05.006
Najavits, L. (2002). Seeking safety: A treatment manual for PTSD and substance abuse. Guilford Publications.
Narayan, A. J., Englund, M. M., & Egeland, B. (2013). Developmental timing and continuity of exposure to interparental violence and externalizing behavior as prospective predictors of dating violence. Development and Psychopathology, 25(4, pt1), 973-990.
National Child Traumatic Stress Network (2015). Complex trauma. http://www.nctsn.org/
Perry, B. D. (2006). Applying principles of neurodevelopment to clinical work with maltreated and traumatized children: The neurosequential model of therapeutics. In N. B. Webb (Ed.), Working with traumatized youth in child welfare (pp. 27-52). The Guildford Press.
Perry, B. D. (2008). Child maltreatment: A neurodevelopmental perspective on the role of trauma and neglect in psychopathology. In T. P. Beauchaine & S. P. Hinshaw (Eds.), Child and adolescent psychopathology (pp. 93-128). John Wiley & Sons Inc.
Petra, M., & Kohl, P. (2010). Pathways Triple P and the child welfare system: A promising fit. Children and Youth Services Review, 32(4), 611-618.
Price-Robertson, R., Bromfield, L., & Vassallo, S. (2010). The prevalence of child abuse and neglect. Australian Institute of Family Studies.
Rathus, J. H., & Miller, A. L. (2014). DBT skills manual for adolescents: Guilford Publications.
Read, J. P., Bollinger, A. R., & Sharkansky, E. (2003). Assessment of comorbid substance use disorder and posttraumatic stress disorder. In P. Ouimette & P. J. Brown (Eds.), Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders (pp. 111-125). American Psychological Association.
Rosenman, S., & Rodgers, B. (2004). Childhood adversity in an Australian population. Social Psychiatry and Psychiatric Epidemiology, 39(9), 695-702.
Salloum, A., Kondrat, D. C., Johnco, C., & Olson, K. R. (2015). The role of self-care on compassion satisfaction, burnout and secondary trauma among child welfare workers. Children and Youth Services Review, 49, 54-61.
Sanders, M., Markie-Dadds, C., & Turner, K. (2003). Theoretical, scientific and clinical foundations of Triple P-Positive Parenting Program: A population approach to the promotion of parenting competence. The Parenting and Family Support Centre.
Sanders, M. R., Pidgeon, A. M., Gravestock, F., Connors, M. D., Brown, S., & Young, R. W. (2004). Does parental attributional retraining and anger management enhance the effects of the Triple P-Positive Parenting Program with parents at risk of child maltreatment? Behavior Therapy, 35(3), 513-535.
Scheeringa, M. S., Myers, L., Putnam, F. W., & Zeanah, C. H. (2015). Maternal factors as moderators or mediators of PTSD symptoms in very young children: A two-year prospective study. Journal of Family Violence, 30(5), 633-642.
Sheehan, R. (2019). Cumulative harm in child protection: The hidden concern. Australian Social Work, 72(4), 434-446.
Sheridan, M., & Nelson, C. A. (2009). Neurobiology of fetal and infant development. In C. H. Zeanah (ed.), Handbook of infant mental health (3rd ed., 40-58). The Guildford Press.
Skinner, B. F. (1972). Humanism and behaviorism. The Humanist, 32(4), 18-20.
Spratt, E. G., Friedenberg, S. L., Swenson, C. C., LaRosa, A., De Bellis, M. D., Macias, M. M., Summer, A. P., Hulsey, T. C., Runyan, D. K., & Brady, K. T. (2012). The effects of early neglect on cognitive, language, and behavioral functioning in childhood. Psychology, 3(2), 175-182. https://doi.org/10.4236/psych.2012.32026
Swenson, C. C., & Schaeffer, C. M. (2014). MST-CAN: An ecological treatment for families experiencing physical abuse and neglect. In S. Timmer & A. Urquiza (Eds.), Evidence-based approaches for the treatment of maltreated children: Considering core components and treatment effectiveness (pp. 237–257). Springer Science + Business Media. https://doi.org/10.1007/978-94-007-7404-9_13
Sylvestre, A., Bussières, È.-L., & Bouchard, C. (2016). Language problems among abused and neglected children: A meta-analytic review. Child Maltreatment, 21(1), 47-58.
Teicher, M. H., & Samson, J. A. (2016). Annual research review: Enduring neurobiological effects of childhood abuse and neglect. Journal of Child Psychology and Psychiatry, 57(3), 241-266.
Thompson, R. A. (2016). What more has been learned? The science of early childhood development 15 years after neurons to neighborhoods. Zero to Three Journal, 36(3), 18-24.
World Health Organization. (2006). Preventing child maltreatment: A guide to taking action and generating evidence. World Health Organization.
Author information
Govind Krishnamoorthy, PhD, University of Southern Queensland
Dr. Krishnamoorthy is a clinical psychologist and senior lecturer in the School of Psychology and Wellbeing at the University of Southern Queensland. He has worked for over a decade in both public and private sectors offering child and adolescent mental health services. As a co-developer of the Trauma Informed Positive Behaviour Support (TIPBS) program, Dr. Krishnamoorthy’s research and clinical experience has focused on addressing the social emotional needs of children and adolescents impacted by child maltreatment.
Kay Ayre, EdD, Edith Cowan University
Dr. Ayre is a lecturer in Early Childhood Studies in the School of Education at Edith Cowan University Western Australia. She worked for the Queensland Department of Education for thirty-two years as a classroom teacher in the early years, a deputy principal Early Years, an advisory visiting teacher in behaviour and a behaviour team leader. Dr. Ayre has worked extensively with disengaged and disruptive children, their teachers, and schools. Her research and her teaching focus on challenging behaviour of children includes those impacted by trauma, trauma-informed positive behaviour support, functional behaviour assessment and childhood wellbeing and resilience.
Bronwyn Rees, MClinPsych, Young Minds Psychology
Ms. Rees is a Clinical Psychologist with over 20 years of experience in working with children, adolescents and their families with mental health concerns and living with chronic and/or complex medical conditions. She has worked in a range of settings in both the public and private sectors including child and youth mental health services, paediatric and adult health services and in private practice.
Samantha Brown, DPsych, University of Southern Queensland
Dr. Brown is a clinical psychologist and lecturer in the School of Psychology and Wellbeing at the University of Southern Queensland. She has 20 years of experience working with children and their families in community and public health settings. She is the Program Director for Postgraduate Psychology and has a training and research interest in complex trauma.

